“Foreign body–fishhook.” We commonly see these injuries in our emergency departments and think, “This could be a real pain to remove from wherever it may be.” Sometimes we need a simpler method, or even a MacGyver-like alternative to make our jobs easier, so our days spent in the trenches are more like our days wetting a line.
Explore This Issue
ACEP Now: Vol 35 – No 06 – June 2016The Case
A 35-year-old, right-hand dominant, previously healthy male presents with a fishhook lodged in his right first digit. The injury occurred that morning, the opening day of trout season. His buddy tried meticulously to dislodge the hook to no avail. The patient now presents with finger pain and an inverted smile, and he is anxious to get back to that game of cat and mouse with an elusive nine-pounder that’ll win him a $250 gift card for the local tackle shop.
Background
Most fishhooks become embedded in either the hand or face. Unfortunately, some fishhooks will find their way into people’s eyes or even intracranially, as described in a case report in 1992.1,2 Obviously, ophthalmology will need to be consulted for ocular fishhook injuries, but the remaining majority of these occurrences can be dealt with in the emergency department.
Having the patient describe or even draw a picture of the fishhook will help the clinician decide which of the following techniques may be most appropriate for removal. The smaller size and shape of most recreational fishhooks keep them from penetrating deep into the soft tissue. However, commercial hooks and some sport-fishing tackle can be much larger and could very well access deeper neurovascular or bony structures. While not required for these accidents, radiographs can help identify the type of fishhook (eg, single-barbed, multi-barbed, treble), the size of the hook, its orientation within the soft tissue, and proximity to bony structures. Theoretically, using a water bath ultrasound technique, the emergency physician could identify nearby neurovascular structures that could be damaged when attempting to remove the hook. In that case, surgical colleagues should be consulted.3 Also consider consultation of a specialist when other vital regions (eg, joints, tendons, testicular, urethral, or peritoneal) are involved.
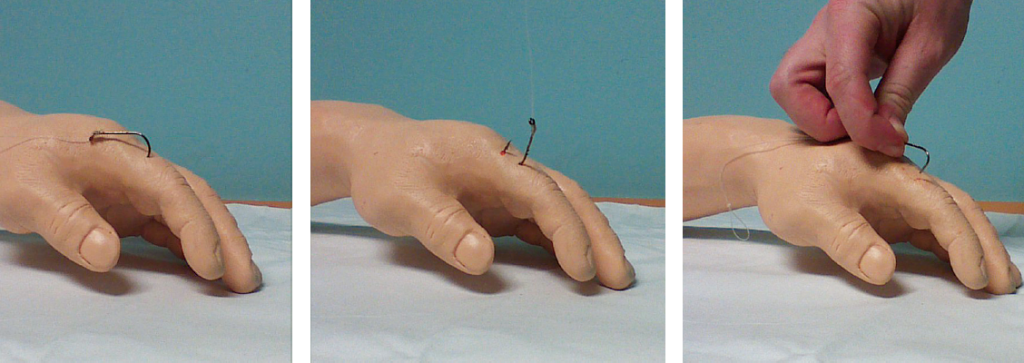
Classically, there are three different techniques that are used to remove embedded fishhooks: pull through, barb sheath, and string yank. There is a simple retrograde technique that is often attempted by the patient in the field prior to arrival. This technique is just as it sounds and is often only successful for very superficial hook injuries. As far as we know, there is only one prospective study that has reported success rates of these different fishhook removal techniques.1 In 1990, Doser et al evaluated 97 fishhook injuries that occurred in Alaska. They reported the greatest success rate (56/97, 58 percent) with the advance-and-cut technique when compared to all the other approaches. While the success rate was higher, they suggest attempting less traumatic retrograde techniques prior to progressing to advance and cut. Of the 87 injuries that were followed up, none had any complications or subsequent infections, despite the fact that only five patients were placed on prophylactic antibiotics.1
Pages: 1 2 3 4 | Single Page






No Responses to “Emergency Medicine Techniques, Equipment List for Removing Fishhooks Lodged in Patients”