Explore This Issue
ACEP Now: Vol 36 – No 01 – January 2017ILLUSTRATION: Chris Whissen & shutterstock.com
The laryngeal mask is, in fact, the only gravity-enhanced ventilation device. Gravity and loss of tone defeat the face mask. Conversely, administration of propofol, which induces a deep loss of upper-airway tone, is far and away the most commonly used medication for laryngeal mask anesthesia. The loss of tone in a supine position is ideal for creating the laryngeal mask seal around the bowl of the device. The soft tissues of the upper airway (base of tongue, epiglottis, and perilaryngeal structures) collapse backward onto the bowl of the LMA as muscular tone about the mandible is abolished.
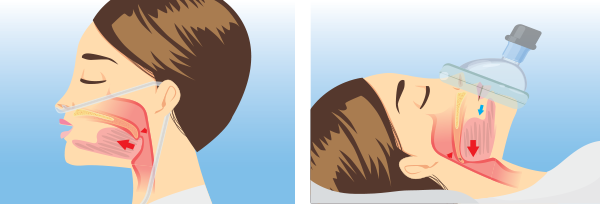
In addition to the ergonomic challenges of doing effective mask ventilation—trying to create a face seal while pressing against the face but pulling up on the mandible simultaneously—there are many physiologic reasons why mask ventilation in a flat position is bad for oxygenation and also why it has a high risk for regurgitation. As a face mask is squeezed over the mouth, the oropharynx gets pressurized (see Figure 1). The goal is to have air only go into the lungs as opposed to the collapsed esophagus. Unfortunately, as pressure increases, especially at about 20 cmHg, air will enter the esophagus and subsequently the stomach. This insufflation of the stomach then leads to regurgitation of stomach contents back up the esophagus to the perilaryngeal area of the hypopharynx (at the top of the esophagus). Regurgitation risk is dramatically increased by having the patient’s stomach and head on the same level or, in an obese patient, the stomach higher than the mouth when the patient is supine. As the stomach gets insufflated, gravity promotes regurgitation of stomach contents into the upper airway.
The LMA, in contradistinction to a face mask, provides some isolation of the esophagus and larynx. The tip of an LMA-type device wedges into the upper esophagus. It’s not a complete isolation like a cuffed tube in the trachea, but by “corking” the top of the esophagus, there is some protection from gas entering the esophagus. Additionally, the bowl of the LMA is sitting directly under the laryngeal inlet, so the amount of pressure needed to get oxygen into the lungs is less than what is used typically with a face mask, having to start from outside the mouth and flow around the tongue.
Pages: 1 2 3 4 | Single Page






3 Responses to “Should Emergency Physicians Abandon Face-Mask Ventilation?”
January 30, 2017
Jose Dionisio Torres, Jr., MDWhat do we have is cost and demand? And the illusion of patient safety.
The public doesn’t know the difference from a bvm..and and lma/or king lt.
These devices are better in ventilation than bvm. But need the bvm if there is a contraindication.
Facemask cheaper but ensures air will go into the stomach ensuring higher risk of aspiration. But don’t use in Coffin position described by you Dr. Levitan. Ramp them up as high as possible if bvm is to be used.
Thank you for the Post Dr. Levitan.
Thank you Mr. Robert Ackerman on sharing this post with me.
March 5, 2017
Craig NavarijoI believe the bvm can be made much more safely than it is today…
in fact, I have working protoypes of a bvm that an individual can selectivley limit volume delivery with.
and that makes maintaining a seal extremely easy ….
March 6, 2017
Steve LeCroyDr. Levitan,
Would you consider using one or two NPA’s like naso-flo that can provide supplemental oxygen along with CPAP instead of a cannula and non-rebreather mask?