Evolving to Meet the PPE Need
The work of #GetUsPPE has evolved in the weeks since it started, as its volunteers began to understand the true complexity of the issues.
Explore This Issue
ACEP Now: Vol 39 – No 05 – May 2020There have essentially been three phases of the effort. The first was handling small public donations of PPE from individual people with supplies in their basements or laboratories. The second phase involved working with domestic manufacturers and makers working quickly to produce some kinds of PPE in the United States. The third, Dr. He explained, has involved building algorithms to maximize PPE distribution once the international supply chain functions again.
“This is not what I planned to spend my months of March and April doing,” said Dr. Ranney, who is also a public health researcher. “I have never worked on supply chain issues before, but I couldn’t just sit by and watch my colleagues be put at risk.”
By now, Dr. He said he feels like he has “basically obtained a PhD in supply chain management” in a matter of weeks.
“I’ve had quite the learning experience about PPE,” he added. “Why is an N95 [respirator] different from a KN95? Why is there a difference in manufacturing processes? Why does a hospital need one type of PPE and nursing homes need others? It’s a mixing and matching of problems.”
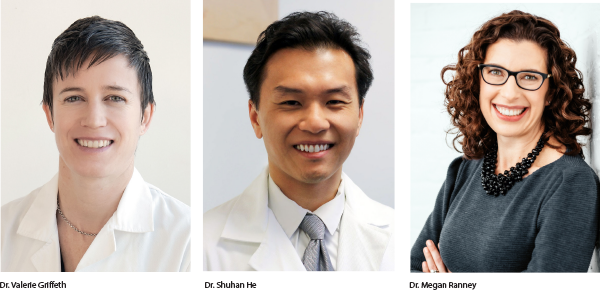
One measure of the effort’s success, said Valerie Griffeth, MD, PhD, an emergency physician soon moving to Advocate Health Care in Chicago, can be found in the way conversations have recently shifted with respect to PPE.
“I think we have made significant progress and, in a sense, that’s reflected in the fact that PPE has become secondary to the story about testing and reopening the economy,” she said.
However, it’s “absolutely disappointing” that #GetUsPPE and other grassroots efforts, such as Project N95, have had to fill the void left behind by what she sees as a government that’s been slow to act.
In late January and into early February, Dr. Griffeth was in the midst of job interviews and her partner expressed some concern about her risks while traveling. Dr. Griffeth began looking into Centers for Disease Control and Prevention (CDC) guidance and gathering as much information as she could find about SARS-CoV-2 (called, at that point, 2019-nCoV), the novel coronavirus that causes COVID-19.
On Feb. 6, she said, the CDC posted guidelines recommending that health care workers don respirators when working with patients with respiratory symptoms. But on March 10, the CDC revised those guidelines to suggest health care workers wear simple surgical masks instead of respirators because of anticipated shortages.
“The CDC in this case got things wrong,” said Dr. Griffeth, who got involved as co-founder of #GetUsPPE after co-authoring a letter advocating for the protection of frontline workers. “This is something we saw coming and we could have prevented it if we’d taken more drastic measures.”1
While Dr. Ranney and Dr. He have been involved in supply chain issues, Dr. Griffeth has been doubling down on her advocacy.2 “I’ve been networking with politicians and grassroots organizations,” she said. “As physicians, we have a voice that people listen to and that’s true now more than ever. This pandemic has really raised our ability to get connected not just to state representatives but also to national representatives. People are taking our phone calls when, in the past, they may not have, so there’s been a lot of value in that.”
Pages: 1 2 3 4 | Single Page





No Responses to “Emergency Physicians Are Taking the Lead to #GetUsPPE”