Audience: I learned in business school there’s no such thing as a merger. They are always acquisitions. My question is, what are you seeing, and are there any activities about expansions beyond the usual SNF-ist [skilled nursing facility], hospitalist, acute care model to partnering?
Explore This Issue
ACEP Now: Vol 35 – No 03 – March 2016JK: We have a task force on alternative payment models. With the whole concept of bundled payments, we think they are going to carve out emergency medicine, and I think the carve out is going away sooner than we expected. [Editor’s Note: See page 16 for a 2016 update on bundled payments.]
If you’re an owner, hopefully you have a voice. If you’re in a group where you’re not an owner but they have a culture of including physicians and they invite your opinions, then you should give them and ask for information. The other thing you should do is check your employment agreement. There may be protections or considerations included. —Ray Iannaccone, MD, FACEP
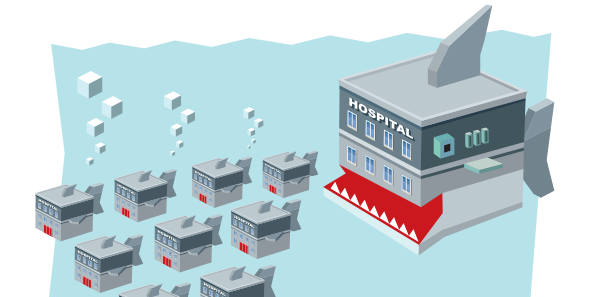
RI: Over the last five to seven years, we’ve gone from a situation where hospital administrators would never consider putting more than one service line under one contract to the exact opposite.
SB: We’re seeing that universally across the market. Hospital CEOs will say, “You’ve done such a great job in the ED. Will you take a look at the hospitalists? Can you take a look at cardiologists?”
RM: I’m going to tell you from my days in capitated care that when the pie gets smaller, the table manners change.
Audience: A large part of our income comes from private insurance companies, and there are high-profile planned mergers of four of the five largest insurers in the United States. What is the marginal value of private for-profit health insurance vis-à-vis a public payer like Medicare?
JK: The term health insurance company is an oxymoron because health insurance companies do not exist for the health of their patients and their clients. They exist to make profits for their shareholders. We need to go after the insurance companies and have them show their true colors as best we can, and we need to ally with our patients.
Audience: I’m representing the Section on Medical Humanities. This was not a very humanistic discussion, not much poetry, but my question is actually concerning what happens to academic medical centers [AMCs] in all of these changes. AMCs are more expensive than typical community hospitals. My question is, what’s the role of emergency medicine in helping academic medical centers to successfully navigate some of the changes that are coming down the road?





No Responses to “Emergency Physicians Discuss Mergers, Money, Future of Emergency Medicine at ACEP15 Council Town Hall”