BA: There will be fewer AMCs, and that’s a larger dilemma for the educational needs of the country than it is for the clinical needs of the country. Community systems that can partner with AMCs on an educational mission are going to be needed. I don’t know that all of the AMCs we have currently are going to be needed for the quaternary needs of the population. In emergency medicine, we’re systems experts. To the degree that we can help strengthen those community and academic partnerships in our markets, that’s the area that’s going to help academic medicine the most.
Explore This Issue
ACEP Now: Vol 35 – No 03 – March 2016RM: Academic hospitals lose money on teaching, they lose money on research, and they have very high fixed costs. They have a problem.
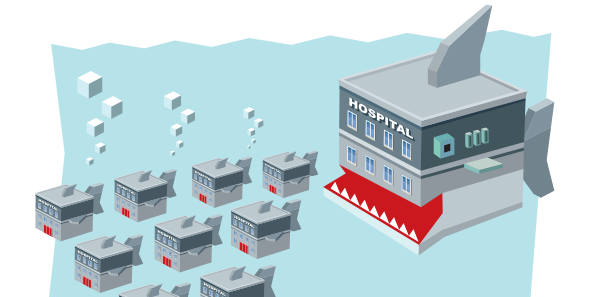
Audience: The evidence that I’ve seen out there suggests that consolidation raises prices. It may decrease costs, but those costs are often pocketed by the institutions they’re consolidating, and there’s very little evidence the consolidated institutions actually have increased quality. I’m wondering what the case is for the nation and for our patients to encourage consolidation under those circumstances.
BA: These are market forces, and you’re not going to be able to stop the market forces from doing it. Your points are well taken. The successful consolidations will be those that are able to lower total cost of care for populations and be able to tell a quality and value story associated with it. Having the infrastructure to do this new work is so expensive. We’ll spend $30 million next year on care management, IT, analytics, new resources, clinical pharmacists, call centers, and data aggregation tools to try to be successful in a population health framework. You can’t duplicate that without having scale.





No Responses to “Emergency Physicians Discuss Mergers, Money, Future of Emergency Medicine at ACEP15 Council Town Hall”