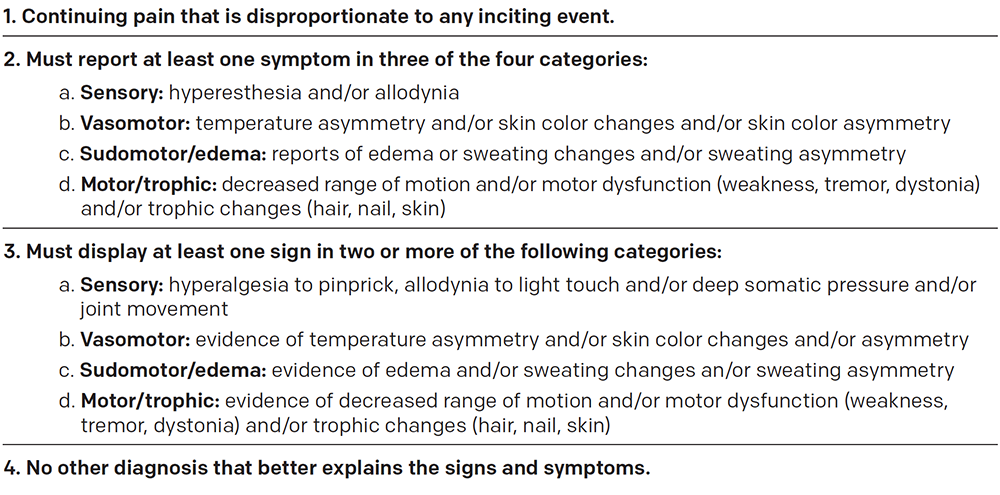
The diagnosis of CRPS has historically been one of exclusion. The Budapest criteria were established in 2003 to objectively diagnose CRPS and have been shown to have a sensitivity of 99 percent and a specificity of 79 percent.6 These four criteria must be met for the diagnosis: 1) pain out of proportion to the inciting injury; 2) patient’s reported history of at least one symptom in three of the four categories of sensory (eg, hyperesthesia, or increased pain response to a mildly painful stimulus, and allodynia, or a painful response to a nonpainful stimuli), vasomotor changes (eg, temperature or skin color asymmetry), sudomotor/edema changes (eg, asymmetric limb edema or sweating), and motor/trophic changes (eg, decreased range of motion; weakness or atrophy; tremor; or hair, nail, or skin changes); 3) the clinician’s own observation of at least two symptoms that fall into two of the previously mentioned categories; and 4) no other explanation for the patient’s symptoms (see Table 1).
Explore This Issue
ACEP Now: Vol 35 – No 12 – December 2016Treatment
Several treatment options are available. There is evidence for posttraumatic inflammation in CRPS, so nonsteroidal anti-inflammatory drug or steroid therapy in the acute stage is reasonable. A high dose of prednisolone has been proposed as therapy.6 Additional oral medications that can be used include tricyclic antidepressants and anticonvulsants such as gabapentin and carbamazepine. There is some evidence that gabapentin or carbamazepine therapy may reduce pain in CRPS.6 Bisphosphonates inhibit the activity of osteoclasts. Pamidronate 60 mg as one intravenous dose has been proposed.9,10
Topical dimethyl sulfoxide (DMSO 50 percent cream) has been shown to have a positive effect on pain, presumably through its role as a free-radical scavenger. Applied for two months, it may provide significant pain relief.10 Other topical medications such as capsaicin, lidocaine 5 percent, or eutectic mixture of local anesthetics (EMLA) cream may be used as well. Patients should be encouraged to use the affected extremity. Specifically, splints, slings, and immobilizing devices, particularly for prolonged periods, should be avoided.9
Intravenous immune globulin has been used effectively, with the rationale that CRPS is related to the presence of unidentified neural antibodies. However, use in the emergency setting has not been recommended.11 The role of opioids as a second- or third-line option for therapy (“rescue dosing”) has not been completely defined. Opioids have not been recommended, except with specific advice and input from a pain management specialist.9 There are concerns for tolerance, cognitive impairment, and opioid-induced hyperalgesia.6 Non-pharmacologic treatment options include appropriate physical and occupational therapy regimens such as isotonic strengthening, passive gentle range of motion, aerobic conditioning, aquatic therapy, and ergonomics.
Pages: 1 2 3 4 | Single Page




No Responses to “What Emergency Physicians Need to Know About Complex Regional Pain Syndrome”