End-tidal capnography has gained momentum over the years as a standard for monitoring patients undergoing procedural sedation in the emergency department, with a level B recommendation coming out of ACEP’s clinical policy regarding procedural sedation in 2014.1 It can identify hypoventilation earlier than other monitoring tools we have at our disposal in the emergency department, but its utility doesn’t end there. It can quickly and efficiently answer clinical questions beyond that of sufficient ventilation. Are the chest compressions being performed on your cardiac arrest inadequate? Should you stop resuscitation efforts? Is your hyperglycemic diabetic in diabetic ketoacidosis (DKA)? Is that nasogastric tube in the stomach? End-tidal capnography can lend insight to these questions that emergency physicians encounter on a daily basis. End-tidal carbon dioxide (EtCO2) sensibly correlates with the pathophysiology of those and many other disease processes and can help guide decision making on your next shift.
Explore This Issue
ACEP Now: Vol 35 – No 11 – November 2016Capnography offers an indirect method to detect metabolic acidosis. EtCO2 measurements have been shown to closely estimate arterial partial pressure of carbon dioxide (pCO2) in healthy patients and also in the presence of metabolic derangements such as acidosis.
Understanding the Capnogram
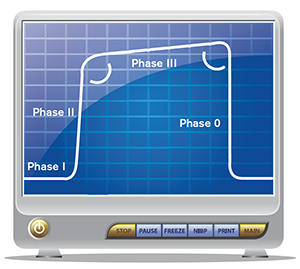
Figure 1. Normal, healthy capnogram.
The end-tidal capnogram is separated into four separate phases (see Figure 1). Phase 0 begins during the inhalation phase of the respiratory cycle and the capnogram drops precipitously from its peak level at the end of expiration. Once the patient begins to exhale (phase I), the initial expired air is predominantly dead space with little expired carbon dioxide (CO2), but as the more densely concentrated CO2 is expired, there is a sharp increase in the end-tidal waveform that represents phase II. The waveform then plateaus during phase III, with slight increases in the CO2 concentration from alveolar air. The discrete end-tidal number we refer to is the value at the end of phase III, the very end of expiration prior to inhaling the next breath. Depending on the situation, the actual waveform of the capnogram and/or the end-tidal value at the end of exhalation may help us with more than just determining hypoventilation in patients undergoing procedural sedation in the emergency department. (See our September 2015 article, “How to Use End-tidal Capnography to Monitor Asthmatic Patients,” at www.acepnow.com/article/how-to-use-end-tidal-capnography-to-monitor-asthmatic-patients for more information on using capnography and for a detailed review on using capnography to evaluate asthmatic patients.)
A New Breathalyzer for Detecting DKA?
It’s nearing the end of your shift when you sign up for your last patient of the day. This fast-breathing diabetic had been sitting in Fast Track for a leg infection, and when the glucometer flashed “HIGH,” he was moved to your higher-acuity area for more workup. You cringe as you picture the needle puncturing his wrist for an arterial blood gas (ABG) test and wonder whether you’ll be breaking out that insulin drip. DKA is an endocrine emergency hallmarked by hyperglycemia, ketonemia, and metabolic acidosis. Ma et al demonstrated that knowledge of the arterial pH in suspected DKA added little to clinical gestalt and altered the emergency physician’s management in only 2.5 percent of cases.2 Do we even need to subject our patients to this test? Although the pH of the often less painful venous blood gas has been shown to be comparable to that of an arterial blood gas, you wish you had an even quicker noninvasive screening tool.3
Pages: 1 2 3 4 | Single Page




No Responses to “End-Tidal Capnography Can be Useful for Detecting Diabetic Ketoacidosis, Monitoring COPD”