Explore This Issue
ACEP Now: Vol 34 – No 05 – May 2015References
- Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007;38(3):967-973.
- Smith WS, Sung G, Starkman S, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke. 2005;36(7):1432-1438.
- Smith WS, Sung G, Saver J, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke. 2008;39(4):1205-1212.
- Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914-923.
- Ciccone A, Valvassori L, Nichelatti M, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med 2013;368(10):904-913.
- Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 2013;368(10):893-903.
- Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372(1):11-20.
- Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019-1030.
- Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018.
- Saver J, Goyal M, Bonafe A, et al. Solitaire FR with the intention for thrombectomy as primary endovascular treatment for acute ischemic stroke. American Heart Association International Stroke Congress, Feb 2015; Nashville, Tenn.
- Paciaroni M, Inzitari D, Agnelli G, et al. Intravenous thrombolysis or endovascular therapy for acute ischemic stroke associated with cervical internal carotid artery occlusion: the ICARO-3 study. J Neurol. 2015;262(2):459-468.
Pages: 1 2 | Single Page






5 Responses to “Endovascular Intervention for Stroke May Become Alternative to tPA”
May 24, 2015
Arno Vosk, MD, FACEPWe all hope this treatment really works. With practically all such things, though, the evidence supporting it comes from sources with a vested interest. The author seems aware of this.
Unanswered questions that occur to me right away: What are long-term results? Where does skill of the operator factor in? What exactly are criteria for patients who might benefit?
We are all desperate for a treatment for stroke that works, but this desperation should not cloud our judgement, or make us overeager to espouse new treatments that might not actually work well, or might not be safe. Alas, most of the information in situations like this comes from tainted sources.
May 24, 2015
Edward JauchIn the title the author misses the point of the trials referenced. The recent trials have largely compared IV to IV + endovascular thrombectomy. IV tPA will remain recommended as first line therapy and IA approaches recommended for those who meet criteria largely used in the recent stent-retriever studies, typically after receiving IV tPA. IA should not be considered as an alternative for IV tPA.
May 26, 2015
Ryan RadeckiHi Edward –
I’m afraid the editors have mis-titled my submission – I agree with your statement the trials did not evaluate IA intervention as an alternative to IV tPA. Upcoming trials appear to be addressing such a hypothesis, but the current trials are largely IA + IV tPA. The title given to the online version here makes such an allusion not referenced anywhere in the body of my article.
– Ryan
May 24, 2015
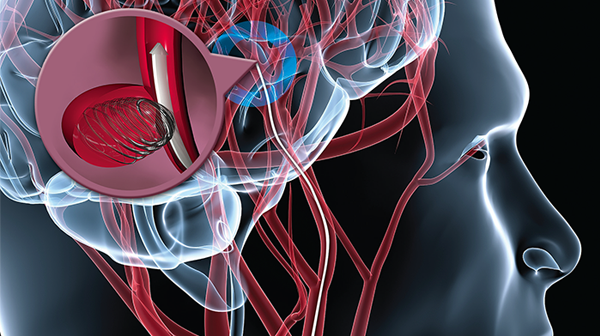
Edward JauchBy the way, among the inaccuracies in the blog, the picture is cool but demonstrates coiling an aneurysm and not related to treating an acute ischemic stroke.
June 1, 2015
Stroke DocRe: IV tpa:
“In the largest meta-analysis of angiographically confirmed intracranial occlusions, sustained early recanalization was achieved with tPA only 46.2 percent of the time.1 Comparing this with the observed 24.1 percent spontaneous recanalization rate, tPA clearly has a maximal ceiling for benefit if only one in five additional patients achieved reperfusion.”
“Because one of the best-kept secrets about tPA, the “clot buster,” is that it doesn’t bust clots” is a strange way to begin the preceding paragraph. By your own admission tPA does bust clots, 46.2% over 24.1%, which is actually an impressive difference, although certainly less than what we want.
Points raised about premature stopping of trials may well be good ones, but with now 5 positive (MRCLEAN, ESCAPE, EXTEND-IA, SWIFT-PRIME, REVASCAT) endovascular trials I don’t think it is possible to doubt that acute recanalization is a good idea in ischemic stroke in appropriate patents…and in fact these results actually reinforce my faith in tpa (and its positive Lancet/Cochrane meta-analyses of use < 4.5 hrs), as tpa does the same thing as a stent retriever, just (notably) not as well. (But still better than placebo, with no change in death rate at 3 months.)
I completely agree, however, that we could have resolved the whole tpa controversy a long time ago (including adequate patient subset analysis, which Dr. Radecki has appropriately stressed in previous posts) if someone had repeated NINDS on much larger samples a long time ago. If only.
Two final points…
1) What "recanalization" really comes to clinically depends on several factors – e.g. which artery, what degree of opening (TICI score), when the artery was opened, and what the state of surrounding brain is. As a simple example, the recanalization rate of a proximal MCA occlusion is less than that of an M2. Also, longer clots seem to recanalize more poorly. Note that among the 5 trials better and quicker degree of opening appeared to correlate with better outcomes (weaker results on REVASCAT and MRCLEAN – compare time and TICI 2b/3 recanalization data.)
2) Though the "time is brain" hypothesis has been doubted, it is supported by successive DWI imaging data, and more importantly it must be true in some way for a good number of patients, unless you are willing to believe that the endovascular trials would have produced the same results if the interventionalists had tried to open the relevant arteries the next day instead of within a few hours.
I would like to thank Dr Radecki for his thoughtfulness and non-inflammatory tone…often lacking in these discussions.