
Chronic obstructive pulmonary disease (COPD) is a chronic disease of the lungs caused by inflammatory and structural changes of the small airways and parenchyma of the lungs that result in chronic airflow obstruction and gas trapping. In 2019, the global prevalence of COPD was estimated to be 10.3 percent, and COPD is responsible for about three million deaths per year globally.2,17 COPD is diagnosed by spirometry with a forced expiratory volume in one second to forced vital capacity (FEV1/FVC) ratio of less than 0.7.4 Acute exacerbations of COPD (AECOPD) are a common presentation in emergency medicine. Exacerbations accelerate disease progression and can lead to increased rates of hospitalization and death.4,14 As these exacerbations represent a critical point in the progression of COPD, it is important for emergency physicians to understand the approach to diagnosis and management of AECOPD.
Explore This Issue
ACEP Now: Vol 43 – No 06 – June 2024Initial Evaluation
As with all critical emergency medicine patients, AECOPD patients should be placed on cardiac monitoring and pulse oximetry, and initial evaluation should focus on vital signs and assessment of airway, breathing, and circulation.
History
The history should focus on assessing for the possible trigger, confirming AECOPD, assessing severity of baseline disease, and evaluating for symptoms that may point toward an alternative diagnosis. Common triggers include infections, recent medication changes, colder weather or air pollution, and medication non-adherence. Presenting symptoms of AECOPD include increased shortness of breath, increased frequency of cough, and increased volume of sputum or change in sputum color or consistency. Exacerbations are more commonly caused by viral infections; however, bacterial infections need to be considered. AECOPD associated with purulent sputum production is most commonly due to bacterial infection.
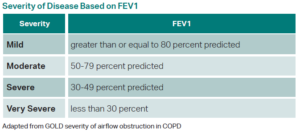
Determining the severity of the patient’s baseline COPD is important in guiding management of the exacerbation. Reviewing the patient’s most recent FEV1, if it is available, is an easy way to determine the severity of obstruction. Other historical items that can assess for severity of disease include history of intubations, frequency of exacerbations and hospitalizations, home O2 flow rate, and comorbidities. Recent hospitalization is important for choosing antibiotic coverage.
And, finally, patients with a history of COPD frequently present to the emergency
department with dyspnea. Although dyspnea in this setting likely represents an AECOPD, other emergent differentials must be considered. Some of the critical differentials include pulmonary embolism, acute decompensated heart failure, pneumonia, pneumothorax, and acute coronary syndrome. Sudden symptom onset suggests pulmonary embolism or pneumothorax. Signs and symptoms of systemic infection (e.g., fevers, chills) suggest pneumonia. Anginal chest pain, chest heaviness, or evidence of fluid overload suggest acute coronary syndrome or acute decompensated heart failure.4,10,11
Physical Exam
Vital sign abnormalities in AECOPD include tachypnea, tachycardia, hypoxemia, and fever if an underlying infection is present. Physical exam should focus on assessment of work of breathing and the cardiopulmonary system. Work of breathing can be assessed by looking for tachypnea, tripoding, accessory muscle use, inability to speak in full sentences, and decreasing level of consciousness. Wheeze and decreased air entry on auscultation are common findings in AECOPD. Focal lung findings (focal rales or dullness to percussion) point more toward pneumonia. Unilateral decreased breath sounds can indicate pneumothorax. An S3 on cardiac auscultation, jugular venous distension, or lower extremity edema suggests heart failure.4,10,11
Pages: 1 2 3 4 5 | Single Page


No Responses to “Evaluating Chronic Obstructive Pulmonary Disease”