The utilization of diagnostic testing in the ED has expanded with the growing number of tools available for electrical testing, imaging, and laboratory analysis. This growth has been questioned by many, especially those who pay for the tests. The conflicts over testing have spilled over into the general media, including a recent opinion piece in The New York Times, written by a cardiologist and a radiologist, that accuses emergency physicians of “ordering multiple CT scans even before meeting a patient.”1
Explore This Issue
ACEP Now: Vol 33 – No 05 – May 2014Why is more diagnostic testing used, and how does it relate to the patient population served? The ED has a critical role as the diagnostic center for the American medical community. Overwhelming amounts of the diagnostics are performed in the ED, particularly related to patients being admitted to the hospital. Because 68 percent of inpatients are processed through the ED, emergency physicians are responsible for a lot of testing and the patient-flow issues related to those decisions. The use of diagnostic testing has markedly changed over the past 20 years with the advent of technology that allows imaging using a broad range of modalities (ultrasound, ionizing radiation, magnetic resonance, positron emissions, and more). These remarkable tools provide unprecedented ability to evaluate patients as they present with a wide range of clinical problems.
What the Data Say
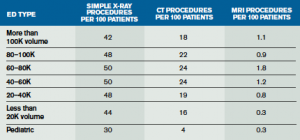
The Emergency Department Benchmarking Alliance (EDBA) data survey is based on performance reports of ED operations, with data from 1,030 EDs that saw 40 million patients in 2012.2 The utilization of diagnostic imaging in the ED is measured in the number of procedures performed per 100 patients seen. The data, reported in cohorts based on type and volume seen in the ED, are in Table 1. There is little difference in use of plain diagnostic X-rays based on volume. There is about a 50 percent difference in CT utilization based on ED volume, with the range only between 16 and 24 procedures per 100 patients. Pediatric EDs only use the CT imaging about four times per 100 patients.
Trauma centers utilize diagnostic imaging to evaluate patients with critical injuries. Within the EDBA data set, the data are analyzed in separate cohorts of trauma centers. Pediatric trauma centers have very different profiles than general EDs, so they are grouped separately. The cohorts exist in hospitals that are Level I and Level II trauma centers, Level III centers, and all other EDs. That analysis shows that the higher-level centers see patient populations with higher acuity, admission rates, EMS arrival, and longer processing times. There are also differences in the use of diagnostics commensurate with the trauma level.
MRI utilization across all EDs has now reached about one procedure per 100 patients, but this increases to 1.8 in the Level I trauma centers.
CT scans are used more frequently in Level I and II trauma centers than in lower-level centers. Emergency physicians in these EDs should be aware of the differences and, when called upon to study their utilization, compare to cohorts at a similar level of trauma designation and pediatric mix. MRI utilization across all EDs has now reached about one procedure per 100 patients, but this increases to 1.8 in the Level I trauma centers. It is critical that emergency physicians are able to understand and use the data on diagnostic testing from their departments and have comparison data available from their peers. The first step to a rational approach to diagnostic-test utilization is to know where you, and others like you, stand. This will allow better decision making by all parties involved in utilization management.
Pages: 1 2 | Single Page







No Responses to “Expanded Diagnostic Testing in the Emergency Department Raises Need for Cohort Data”