
Explore This Issue
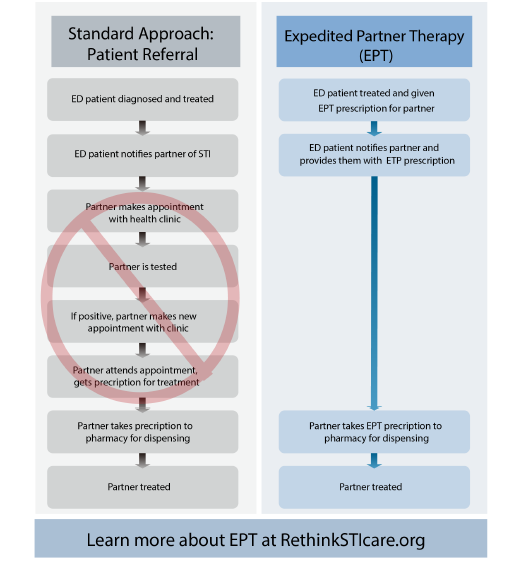
ACEP Now: Vol 40 – No 05 – May 2021Figure 1: Standard therapy versus expedited partner therapy for sexually transmitted infections.
Note that prescribing guidelines vary by state. Some require the name of the patient or partner on the prescription, while in others you can simply prescribe to the name “Expedited Partner Therapy.” Likewise, different states have varying legal requirements regarding what information must be provided along with EPT, such as specific information sheets to hand to the patient.
Once you have confirmed your state supports EPT prescribing, you can take action at a local level. To improve the overall care for STIs, advocate that your department use rapid tests to improve the accuracy of empiric treatment.15 Though EPT can still be offered empirically based on clinical diagnosis before lab confirmation, rapid testing can aid in the precision of selecting which patients should be offered EPT at the primary visit.
Help educate your colleagues and potential prescribers by giving a presentation at your departmental or faculty meetings. Meet with key stakeholders (eg, medical directors, nursing, pharmacy, electronic health record builders, informatics officers, hospital legal counsel, etc.) to determine what orders and policies work best for your group. For patients identified as positive during lab follow-up, work with your medical director and follow-up office (eg, nurse, physician assistant, nurse practitioner, pharmacist, etc.) to create straightforward protocols for offering EPT after lab confirmation. For tips and tools on starting EPT at your emergency department, check out this website designed by emergency physicians: www.RethinkSTIcare.org.
EPT is not a process that will happen on its own in the emergency department. But by learning about EPT and becoming a departmental champion, you can take the critical first step in moving emergency medicine toward improving the sexual and reproductive health of our patients.
 Dr. Solnick is a fellow in the National Clinical Scholars Program at the Institute for Healthcare Policy and Innovation and a clinical lecturer in the department of emergency medicine at the University of Michigan in Ann Arbor.
Dr. Solnick is a fellow in the National Clinical Scholars Program at the Institute for Healthcare Policy and Innovation and a clinical lecturer in the department of emergency medicine at the University of Michigan in Ann Arbor.
 Dr. Fleegler is associate professor of emergency medicine at the University of New Mexico School of Medicine in Albuquerque.
Dr. Fleegler is associate professor of emergency medicine at the University of New Mexico School of Medicine in Albuquerque.
 Dr. May is professor of emergency medicine and director of emergency department antibiotic and outpatient stewardship at UC Davis Health in Sacramento.
Dr. May is professor of emergency medicine and director of emergency department antibiotic and outpatient stewardship at UC Davis Health in Sacramento.
 Dr. Kocher is associate professor in the departments of emergency medicine and learning health sciences at the University of Michigan.
Dr. Kocher is associate professor in the departments of emergency medicine and learning health sciences at the University of Michigan.
References
- CDC estimates 1 in 5 people in the U.S. have a sexually transmitted infection. Centers for Disease Control and Prevention website. Accessed March 3, 2021.
- New CDC report: STDs continue to rise in the U.S. Centers for Disease Control and Prevention website. Accessed March 30, 2021.
- Pearson WS, Peterman TA, Gift TL. An increase in sexually transmitted infections seen in U.S. emergency departments. Prev Med. 2017;100:143-144.
- Batteiger TA, Dixon BE, Wang J, et al. Where do people go for gonorrhea and chlamydia tests: a cross-sectional view of the central Indiana population, 2003–2014. Sex Transm Dis. 2019;46(2):132-136.
- Sexually transmitted disease surveillance 2018. Centers for Disease Control and Prevention website. Accessed April 15, 2021.
- Brackbill RM, Sternberg MR, Fishbein M. Where do people go for treatment of sexually transmitted diseases? Fam Plann Perspect. 1999;31(1):10-15.
- Ware CE, Ajabnoor Y, Mullins PM, et al. A retrospective cross-sectional study of patients treated in US EDs and ambulatory care clinics with sexually transmitted infections from 2001 to 2010. Am J Emerg Med. 2016;34(9):1808-1811.
- St Cyr S, Barbee L, Workowski KA, et al. Update to CDC’s treatment guidelines for gonococcal infection, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1911-1916.
- HHS releases first national strategic plan to address sexually transmitted infections. US Department of Health and Human Services website. Accessed March 30, 2021.
- Ferreira A, Young T, Mathews C, et al. Strategies for partner notification for sexually transmitted infections, including HIV. Cochrane Database Syst Rev. 2013;(10):CD002843.
- Vaidya S, Johnson K, Rogers M, et al. Predictors of index patient acceptance of expedited partner therapy for Chlamydia trachomatis infection and reasons for refusal, sexually transmitted disease clinics, New York City, 2011 to 2012. Sex Transm Dis. 2014;41(11):690-694.
- Legal status of expedited partner therapy. Centers for Disease Control and Prevention website. Accessed March 31, 2021.
- Expedited partner therapy. Centers for Disease Control and Prevention website. Accessed March 31, 2021.
- 2020 ACEP Council resolutions. ACEP Now. 2020;39(12):16.
- May L, Ware CE, Jordan JA, et al. A randomized controlled trial comparing the treatment of patients tested for chlamydia and gonorrhea after a rapid polymerase chain reaction test versus standard of care testing. Sex Transm Dis. 2016;43(5):290-295.
Pages: 1 2 3 4 | Single Page




4 Responses to “Expedited Partner Therapy Can Stop Sexually Transmitted Infections”
June 20, 2021
Gary RobertsTreatment of partners in the setting of STIs is medically appropriate. This article did not address the pitfalls of prescribing medication for an unknown and unseen patient whose medical history cannot be confirmed. Anaphylaxis to cephalosporins is well known and there are numerous medications with potential adverse interactions with azithromycin.
As a physician, I am unwilling to subject an unknown patient to potential harm and am equally unwilling to incur the legal liability attached to an adverse outcome in this situation no matter how noble the cause. (health care equity)
The (potential) patient has the responsibility in this case. ED physicians are neither qualified nor justified to act “in loco parentis” for the community.
June 20, 2021
TWhat if partner has an allergy or adverse drug reaction. You never did a formal evaluation. Is their sovereign immunity?
June 21, 2021
Matt JaegerHow do you propose we prescribe medications to a patient we don’t have a chart for, don’t have a relationship with, haven’t performed a history on, and don’t know what their allergies are? This seem like a risk I’m not willing to take. I don’t think I’m willing to start handing out prescription to unknown individuals.
At some point, patients must take at least partial responsibility for their care and initiate a relationship with a medical provider, be it in an ER, public health clinic, walk-in clinic or a PCP.
June 21, 2021
Gary Roberts, MD, JDWhile “social justice and health equity” are noble motives and lofty goals, the reality of EPT is far more gritty.
Even granting the supposition that there may be some legal protection for the prescribing physician, what protection is there for the unexamined and unseen patient?
Cephalosporins are well-known to have a not insignificant allergic/anaphylactic profile. The myriad potential drug interactions and adverse reactions with doxycyline are well documented.
Nonetheless, the EPT approach is to expose patients to these risks without their consent and lacking any first-hand knowledge of their medical condition.
It is neither the province nor the responsibility of Emergency Medicine to act in loco parentis in these situations. The patient must bear some responsibility.
“Social justice and health equity” in this context is already being well-served. There are numerous free clinics for the treatment of STI.
https://www.yourstdhelp.com/free_clinic_locator.html
Noble motives and the possibility of legal protection are flimsy and totally inadequate excuses to expose unknown patients to significant risks.