Necrotizing Fasciitis Requires Rapid Diagnosis and Treatment
By Kristen Peña, DO; and Sarah Bella, DO, MPH
|
on October 16, 2018
|
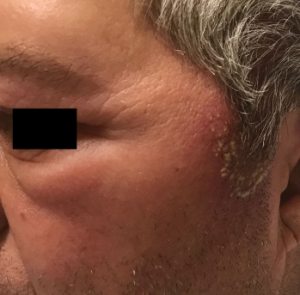
Figure 3: Swelling on the patient’s left eye upper and lower eyelids.

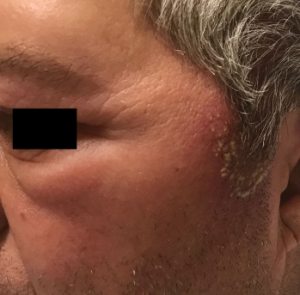
Figure 4: Rash on the patient’s left upper abdomen, similar in appearance to the one on his hand.
Background
Necrotizing fasciitis is a category of soft tissue infection that is described as fulminant deep tissue destruction with systemic signs of toxicity and a high mortality rate.1,2 There are two types of necrotizing fasciitis: polymicrobial (anaerobic and aerobic) and group A Streptococcus.1 Patients typically present with erythema, swelling, pain out of proportion to the exam, crepitus, and skin breakdown with bullae that can begin acutely and rapidly progress and spread.1-3 Risk factors include immunosuppression, drug use, recent surgery, liver disease, traumatic wounds, and diabetes.1-3
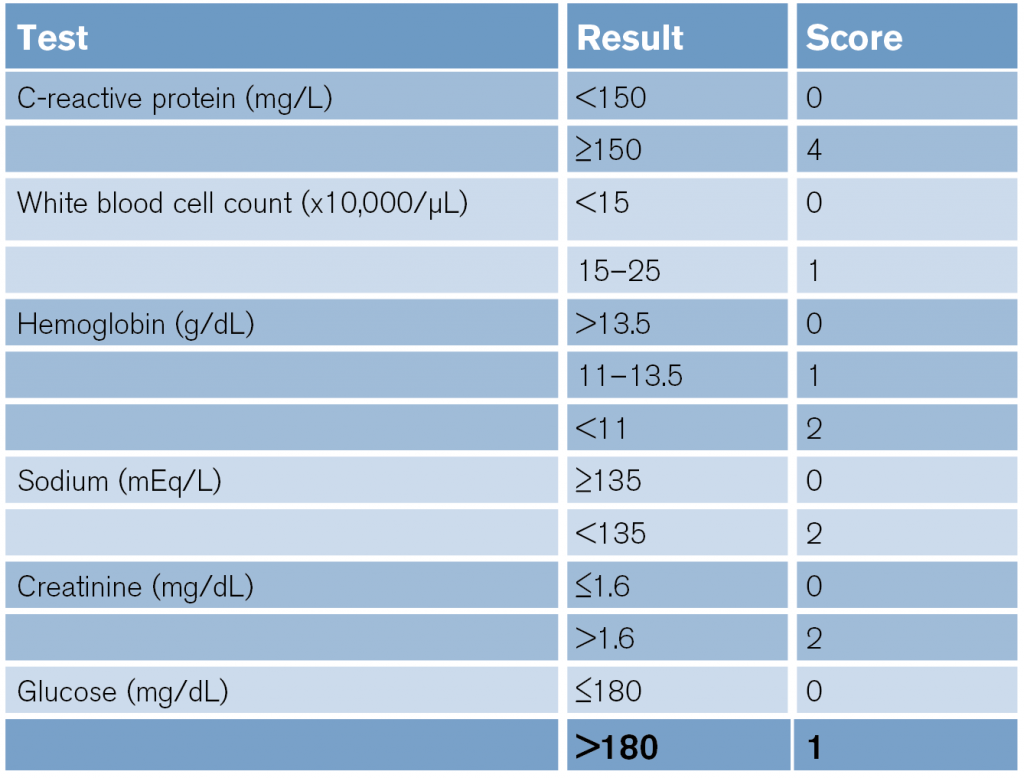
(click for larger image) Table 1: LRINEC Scoring System6
In patients who present to the emergency department with these symptoms and risk factors, it is also important to consider other similarly presenting complications such as acute compartment syndrome (ACS). ACS occurs when fascial compartment pressures surpass capillary perfusion pressures, leading to tissue ischemia and necrosis. ACS is a limb-threatening diagnosis that can occur acutely after fracture or soft tissue injury and requires immediate clinical suspicion and intervention. Both necrotizing fasciitis and ACS are rare diagnoses, and a few case studies have shown that they can occur simultaneously in patients who present with severe extremity pain and signs of a systemic inflammatory response.
To help providers better recognize necrotizing fasciitis in the emergency department, the laboratory risk indicator for necrotizing fasciitis (LRINEC) scoring system was developed based on six laboratory results: total white cell count, hemoglobin, sodium, glucose, serum creatinine, and CRP (see Table 1). Patients with a score of 6 or above should be seriously considered for necrotizing fasciitis.4,5 For example, in the case presented above, the patient’s LRINEC score was 8 for elevated CRP, hyponatremia, and elevated creatinine, which reinforced our suspicion for necrotizing fasciitis and need for emergent treatment.
CT scan is the most helpful imaging modality for detecting necrotizing fasciitis in the deeper soft tissue layers in the emergency department in a timely manner.1,7 However, the only way to definitively diagnose necrotizing fasciitis is surgical exploration and early wound debridement of necrotic tissue.1,7 Surgical exploration should not be delayed, and wound cultures should be obtained. The wound should also be evaluated 24 hours later in the OR and aggressively debrided again if necrotic tissue is present. Broad-spectrum antibiotic therapy should be started and continued until no additional debridement is needed and the patient’s condition improves.7

No Responses to “Necrotizing Fasciitis Requires Rapid Diagnosis and Treatment”