Communication
Explore This Issue
ACEP Now: Vol 39 – No 04 – April 2020Incident command structure should be followed, with centralized communication, messaging, and task delegation, including:
- Identify a liaison to communicate regularly with the local DOH.
- Identify a liaison for communications with the media.
- Identify a COVID-19 hospitalist lead for admissions that are not to the ICU and an intensivist lead for those to the ICU.
- Identify outreach leads for EMS, the homeless and shelter community, SNFs, and jails if your hospital receives these patients.
Stuff
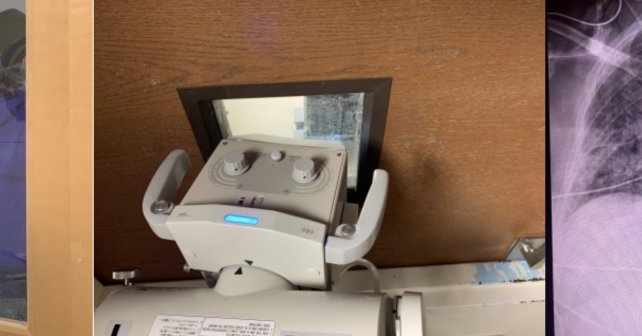
Inventory current amounts of sanitation supplies (especially alcohol-based hand gel and bleach wipes); pulse oximeters; masks, powered air-purifying respirators (PAPRs), and shrouds for PAPR; mirrors for doffing stations; and disposable stethoscopes to anticipate increased needs. We have run short of flu swabs and personal protective equipment (PPE). Consider storing these supplies in ways that prevent hospital personnel and guests from removing them for personal use.
Assess supplies of key medications including antibiotics, sedation, analgesia, neuromuscular blockade, and crystalloid. Plan for use of metered dose inhalers with spacers instead of nebulizers to reduce infectivity.
Establish protocols for handling patient specimens (blood, urine, respiratory viral testing, etc.).
Hospitals should determine how many ventilators are available, including noninvasive positive pressure devices and anesthesia machines; reach out to ambulatory surgery centers for the possibility of using anesthesia machines; and assess the number of extracorporeal life support pumps and circuits available.
Space
Develop a department plan designating which areas of the emergency department will be dedicated to droplet precautions and which areas are negative pressure rooms appropriate to airborne precautions. For areas without an antechamber, consider creating a taped “warm zone” outside of the room for proper doffing. Ensure donning/doffing stations are set up with all needed supplies. Consider taking a photo of the station to post to ensure proper setup. How will you secure these supplies (especially the hand gel and wipes)?
Consider cohorting patients with mild illness who are “patients under investigation” in internal waiting rooms away from well patients or those who could be immunocompromised.
Use phones in the patient rooms to interview noncritically ill patients to reduce trips in and out of the room and to coordinate with nursing or respiratory therapy when they are at the bedside.





No Responses to “Get Your Emergency Department Ready for COVID-19”