In October 2016, the ACEP Board of Directors approved an update of the clinical policy on the evaluation of patients with abdominal pain or vaginal bleeding in early pregnancy. This clinical policy can be found on ACEP’s website, was published in Annals of Emergency Medicine in February 2017, and has been submitted for abstraction on the National Guideline Clearinghouse website. This clinical policy also received endorsement from the Emergency Nurses Association.
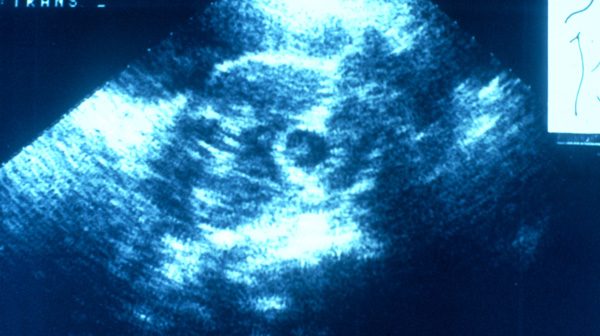
For patients presenting to the emergency department with complications of early pregnancy, the clinician’s primary goal is to localize the pregnancy, if possible, in order to minimize the risk of an undiagnosed ectopic pregnancy. This is of particular concern in this setting because the incidence of ectopic pregnancy in symptomatic ED patients is as high as 13 percent in some series, much higher than the incidence in the general population.1 Performing an ultrasound is a critical part of the evaluation. However, diagnostic algorithms for early pregnancy vary considerably among providers and institutions. Many algorithms still incorporate the principle of the “discriminatory threshold,” typically defined as the level at which the sensitivity of ultrasound is thought to approach 100 percent for the detection of intrauterine pregnancy (if one is present). However, the diagnostic and predictive utility of the β-human chorionic gonadotropin (hCG) level is not as high as once thought. Further, the goal of the emergency department evaluation should be to investigate the possibility of ectopic pregnancy and not solely to identify intrauterine pregnancies, particularly when they are likely to be found. Dissuading the use of ultrasound due to not reaching a discriminatory threshold may lead to misdiagnosis of ectopic pregnancy.
Therefore, the Clinical Policies Committee focused on critical questions about whether the β-hCG should be used to determine the need for an ultrasound and in cases where the ultrasound is indeterminate, whether the β-hCG should be used to predict the risk of an ectopic pregnancy. A systematic review of the evidence was conducted, and the committee made recommendations (A, B, or C) based on the strength of evidence (see Table 1). This clinical policy received internal and external reviews during the 60-day open-comment period. These responses were used to refine and enhance this clinical policy but did not necessarily imply endorsement.
Critical Questions and Recommendations
- Should the emergency physician obtain a pelvic ultrasound in a clinically stable pregnant patient who presents to the emergency department with abdominal pain and/or vaginal bleeding and a β-hCG level below a discriminatory threshold?
Patient Management Recommendations
Pages: 1 2 | Single Page





No Responses to “How to Handle Possible Ectopic Pregnancies in the Emergency Department”