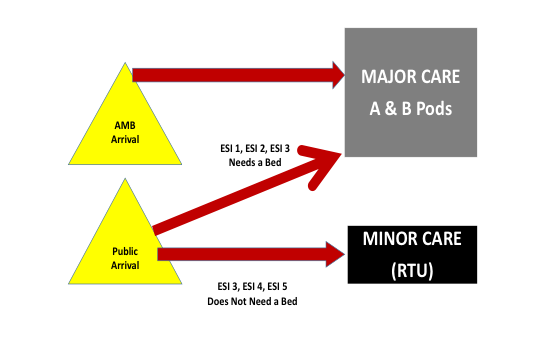
Figure 1: Standardized flow model for Hasbro Children’s Hospital.

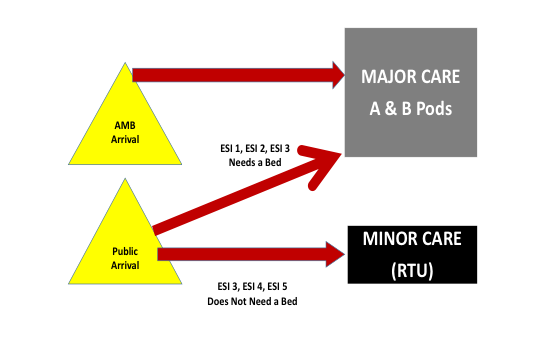
Figure 2: Hasbro Children’s Hospital’s rapid treatment unit rooms.
The results of the change package have impressed the hospital leadership, the stakeholders, and the community (see Table 1).

Table 1: Results of Hasbro Children’s Hospital’s Change Package
The “door-to-doc” times, which had been cut in half with the “Pull to Full” initiative, were reduced even further with the change package. These wait times are settling in at under 20 minutes, something that is hard to do without putting a physician in triage. The overall LOS has come down, particularly the LOS of the RTU, which is consistently well under the 90 minutes goal that was set. The left-without-being-seen rate is now averaging less than 0.5 percent, down from 1.41 percent. Further, the RTU is managing 18 percent of the volume, or 26 patients per day in five treatment spaces. While low acuity patients spent more than two hours in the lower level C Pod, they are now typically in and out in just over one hour.
Topics: EfficiencyEmergency DepartmentEmergency MedicineEmergency PhysiciansPatient CarePatient FlowPediatricsPractice ManagementWorkforceWorkload
About the Author

Shari Welch, MD, FACEP, is a practicing emergency physician with Utah Emergency Physicians and a research fellow at the Intermountain Institute for Health Care Delivery Research. She has written numerous articles and three books on ED quality, safety, and efficiency. She is a consultant with Quality Matters Consulting, and her expertise is in ED operations.
View this author's posts »








No Responses to “Hasbro Children’s Hospital’s “Expedite to Excellence” Project Improve Wait Times and Performance Metrics”