Explore This Issue
ACEP Now: Vol 33 – No 06 – June 2014
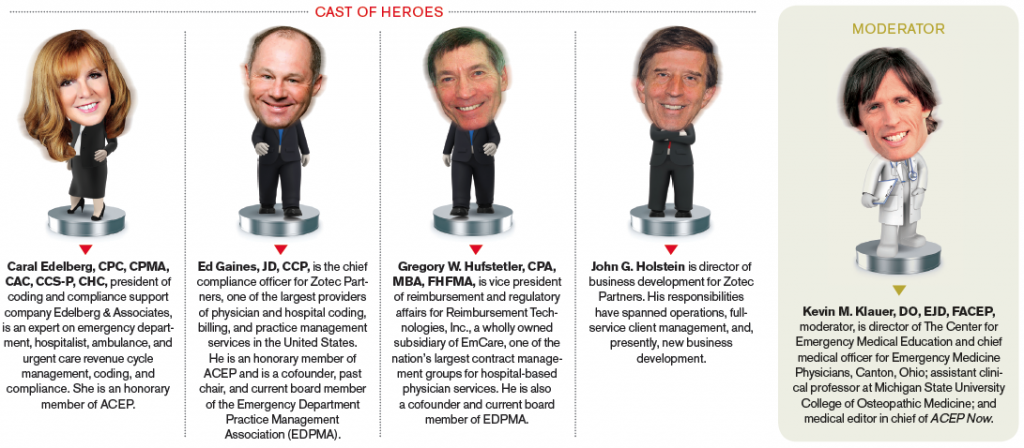
Kevin M. Klauer, DO, EJD, FACEP: What are top challenges in 2014 for health care? Where do we see health care going in 2014? What do you see as non-physicians and executive leaders in emergency medicine?
Ed Gaines, JD, CCP: I think the single biggest challenge we have in health care overall, and specific to emergency medicine, is this “Greatest of Three” formula (GOT) and interim final rules that we have under the Affordable Care Act (ACA) and the Centers for Medicare & Medicaid Services (CMS) regulations. What the commercial health plans are doing, in essence, is using those interim final rules to drive out-of-network (OON) reimbursement to approximately 125 percent of Medicare. Greg Hufstetler has analyzed the EmCare data and found that three of the major health plans—Aetna, Cigna, and UnitedHealthcare— have shifted more then $600 million from the plans to the patients in 2013 using the GOT formula. It really ties to a theme that our CEO and founder Scott Law has talked about. He calls it the great fleecing of the American patient. The plans are paying Medicare plus 20 to 30 percent of the charge, which leaves a significant “balance bill” due from the patient. The balance of the provider charges less the unreasonably low reimbursement by the health plans is being transferred to the patient, and the patient’s having to pay that in states where there isn’t a restriction on balance billing, and that’s a real problem for emergency medicine and all hospital-based specialties. So if we look out over the next five to 10 years, can the emergency medicine specialty exist on a Medicaid- or Medicare-style reimbursement methodology? I don’t think it can exist in the way it does today with independent ED group practices. The recently published Health Affairs study showed reimbursements set to Medicare and Medicaid would produce double-digit losses for most EDs and that historically privately insured patients have subsidized all other ED payer classes.1 With the states that do not have Medicaid expansion, there’s simply not enough reimbursement in the system to pay for the moral imperative, the Emergency Medical Treatment & Labor Act (EMTALA) imperative, and the imperative of emergency medicine to care for all comers to the ED. I think that’s the single biggest challenge we have in EM.





No Responses to “Health Care Professionals Share Insights on Challenges, Future of Emergency Medicine”