
Explore This Issue
ACEP Now: Vol 39 – No 06 – June 2020Smaller emergency departments, or those with lower disease prevalence, might only have a small number of spaces for COVID-19 patients and one room designated for COVID critical care.
High-priority (eg, trauma, stroke, burn, or obstetric patients) and high-risk patients need to move through the screening process quickly and be transported to appropriate critical care areas. Resuscitation areas in COVID hot zones need to process all critically ill COVID-19 patients and any arriving patients with an unknown status. Patients are treated by staff in full PPE, including N95 masks or powered air-purifying respirator, eye shields, gowns, and gloves, who use strict donning and doffing procedures.8
Wearing PPE presents notable challenges. In addition to it being time-consuming to suit up, frontline workers report extreme difficulty in tolerating the warmth of PPE and most can’t withstand full protection from SARS-CoV-2 for more than four hours.
Another strategy includes not allowing staff to float back and forth between hot and cold zones, which exposes patients and staff members to the risk of infection. This will decrease staffing flexibility and impact staffing and workflow on the front lines.
A busy emergency department with higher volume that is part of the epicenter may be able to populate and staff a separate zone for middle- and higher-acuity noncritical patients who need testing and treatments. This will take place in a designated ED care space and may include a lounge chair area. The institution will have to decide whether to take infected patients into imaging suites. Radiology staff will have to provide guidance on appropriate use of plain imaging and high-level scans.
In some cases, having PPE-protected imaging staff take portable films and using plastic-covered portable units is more efficient than cleaning an imaging room between patients. This is even more important in scanning suites, where disinfecting scanners and gantries may take more than an hour. Ultrasound procedures are typically done bedside with disposable sheaths and PPE-protected staff. Health care workers in these areas should wear basic PPE including a surgical mask, eye shield, gown, and gloves.9
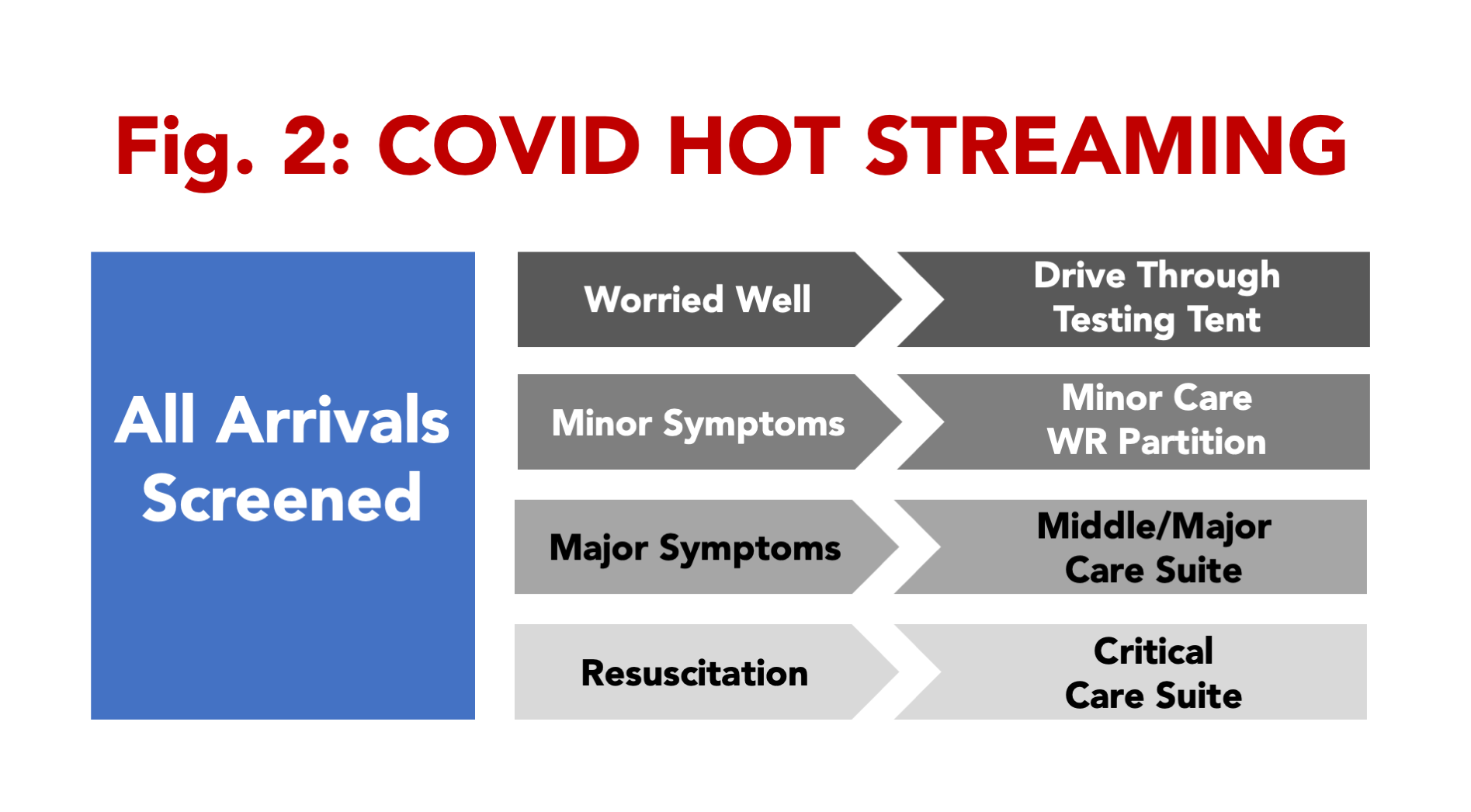
Other arriving patients will have risk factors for SARS-CoV-2 infection but may have low-acuity medical needs and little indication for diagnostic testing. These patients may be best served by evaluation and disposition directly from the intake or screening area. In many emergency departments that have forbidden visitors, the waiting room may serve as a convenient area for minor care.
Take advantage of opportunities to use outdoor spaces and adjacent parking lots, with or without tents, to manage the lowest acuity needs. This includes those who simply need a screening test, those needing a “COVID clearance” to return to work, and the “worried well.” Where drive-through operations can be developed, low-acuity patients could remain in their cars, with self-collected specimens evaluated in a timely manner.
Pages: 1 2 3 4 | Single Page







No Responses to “Help Prevent Coronavirus Spread by Reevaluating ED Flow”