
Explore This Issue
ACEP Now: Vol 38 – No 04 – April 2019Figure 2: Place a Tegaderm film dressing over the patient’s closed eye, gently press out any pockets of air, and apply a copious amount of gel directly over the Tegaderm.
scan, the patient will have to move his or her eyes side to side and up and down to allow complete visualization of the posterior segment.
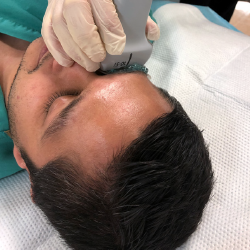
Figure 3: Transverse visualization of the orbit.
Visualize the orbit in both transverse (see Figure 3) and longitudinal planes. After scanning through, the patient should be asked to move his or her eye right to left and up and down. A combination of still images and dynamic scanning clips will best document your exam.
[/fullbar]
References
- Parker C. Optic nerve sheath diameter: window to the soul? Broome Docs website. Accessed Feb. 15, 2019.
- Ohle R, McIsaac SM, Woo MY, et al. Sonography of the optic nerve sheath diameter for detection of raised intracranial pressure compared to computed tomography: a systematic review and meta-analysis. J Ultrasound Med. 2015;34:1285-1294.
Pages: 1 2 | Single Page





No Responses to “High-Yield Ocular Ultrasound Applications in the ED, Part 2”