Part 3 of a 3-part series. Part 1. Part 2.
Common Emergency Department Application
Explore This Issue
ACEP Now: Vol 38 – No 05 – May 2019Structure: Vitreous Humor/Body
Evaluate for: Vitreous hemorrhage, vitreous detachment
The vitreous humor, which goes by several names, is a transparent gelatinous mass that occupies 80 percent of the volume of the eye, filling the space between the lens and the retina. The vitreous is more fluid-like centrally and more gelatinous on its peripheral edges. This vitreous body is surrounded by a collagenous membrane that is in contact with the retina. Because its composition is 99 percent water, a normal vitreous will appear anechoic on ultrasound, giving the posterior chamber a completely black appearance. In the case of vitreous hemorrhage, one will note echogenic material in the posterior chamber (see Figure 1). This increased echogenicity may be obvious or subtle. Woo et al found that the sensitivity of ED physicians utilizing POCUS for vitreous hemorrhage was only 43 percent, but the specificity was 94 percent.1
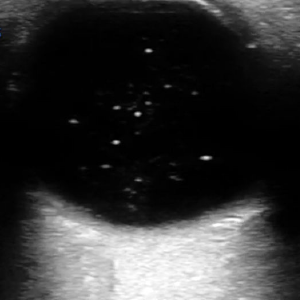
Figure 1: In vitreous hemorrhage, echogenic material is visible in the posterior chamber.
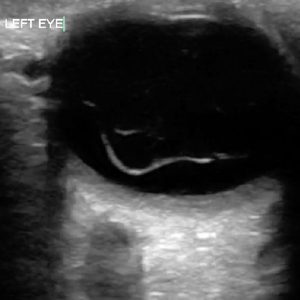
Figure 2: Vitreous detachment may appear similar to a retinal detachment but is more globular and not tethered by any specific structural attachments.
Vitreous detachment is another pathological condition encountered in the emergency department. It occurs when the vitreous membrane separates from the retina and is most often atraumatic. On ultrasound, this may appear similar to a retinal detachment, but a vitreous detachment is more globular and not likely to appear undulating or move along with patient eye movements (see Figure 2). In contrast to the retina, a detached vitreous will not be tethered by any specific structural attachments.
Tips & Tricks: When suspicion is high, increase the ultrasound gain to pick up subtler vitreous hemorrhages.
Ocular ultrasound is easy to learn and can rapidly assess ocular emergencies. With practice, you can easily incorporate POCUS into your diagnostic algorithm and rule in or out important ocular pathology.
Ultrasound Technique
- Explain this bedside procedure to your patient prior to starting. As this is a dynamic

Figure 2: Place a Tegaderm film dressing over the patient’s closed eye, gently press out any pockets of air, and apply a copious amount of gel directly over the Tegaderm.
scan, the patient will have to move his or her eyes side to side and up and down to allow complete visualization of the posterior segment.
- The orbit is a superficial structure. Therefore, a high-frequency linear transducer should be used.
- For comfort and to prevent a mess, place a Tegaderm film dressing over the patient’s closed eye and gently press out any pockets of air. Remember, air is the enemy of ultrasound.
- When performing ocular ultrasound, a copious amount of gel should be used, which will prevent contact of the transducer with the eyelid and minimize direct pressure. The gel can be applied directly over the Tegaderm (see Figure 2).
-
Pages: 1 2 | Single Page





No Responses to “High-Yield Ocular Ultrasound Applications in the ED, Part 3”