Explore This Issue
ACEP Now: Vol 34 – No 07 – July 2015(Click for larger image) Figure 1. Determination of VBM Amount
The Affordable Care Act requires that the Centers for Medicare & Medicaid Services (CMS) apply a value-based modifier (VBM) to Medicare physician fee schedule payments starting with select physicians in 2015 and all physicians by 2017. Unlike the Physician Quality Reporting System (PQRS), which is a pay-for-reporting program that focuses only on quality, the VBM is tied to physician performance on a composite of quality and cost measures. Since 2017 VBM adjustments are based on 2015 performance and apply to group practices of any size, as well as solo practitioners, it is critical that emergency physicians understand how they may be affected by this program.
Quality and Cost Scores
The VBM program scores physician performance based on both quality and cost. Quality is scored under six different quality domains, which ultimately yield a quality composite score. Cost is scored under three different cost domains, which ultimately yield a cost composite score. The quality and cost composite scores are then combined to yield a group’s VBM payment adjustment. Importantly, CMS will not include in its calculations measures for which a group or solo practitioner was attributed fewer than 20 cases. In cases where there is insufficient data, CMS will classify the emergency physician’s performance as “average” for purposes of calculating the composite score (see Figure 1).
The benchmark for each quality measure is based on the national mean of each measure’s performance rate during the year prior to the performance year. The benchmarks for the cost measures are the national mean of performance rates but are further adjusted based on the specialty mix of the providers in the group. Cost measures are also payment-standardized to adjust for geographic differences and risk-adjusted based on patient characteristics.
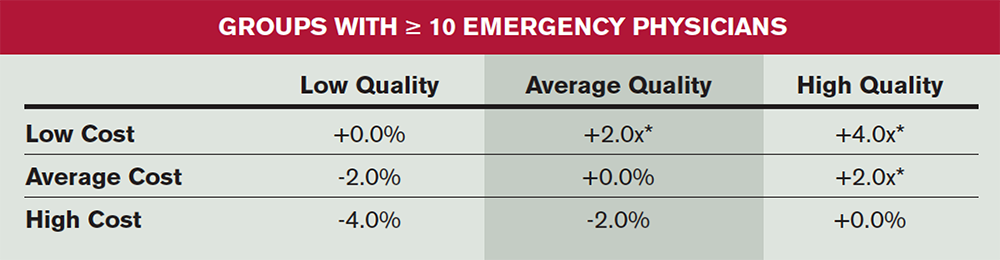
Calculation of the 2017 VBM
CMS will divide the total scores for all physicians into three tiers based on whether they are above, at, or below the national mean. As the program has evolved, CMS has set lower thresholds for smaller groups based on potentially limited group resources. CMS stratifies between groups of >10 eligible providers (see Table 1) and those with two to nine eligible providers and solo practitioners (see Table 2). Of note, eligible providers are defined as all physicians and advanced practice providers, including part-timers and moonlighters, working for the group.
Pages: 1 2 | Single Page






No Responses to “How CMS’ Value-Based Modifier Program May Affect Emergency Physicians”