It is well-recognized that delays in inpatient discharges result in ED boarding of admitted patients. Boarding has a negative impact on ED performance, clinical outcomes, and mortality. Improving the admissions process and decreasing the time patients spend in the emergency department after the decision has been made to admit have a downstream effect on decreasing inpatient length of stay (LOS). Like boarding, discharge delays are associated with increased mortality and adverse events.
Explore This Issue
ACEP Now: Vol 38 – No 10 – October 2019The University Hospital (UHS) in the University of Texas-San Antonio health system had conducted a comprehensive ED improvement project, which dramatically improved door-to-doctor (D2D) times and LOS. Walkaways were reduced, and patient satisfaction soared as the timeliness of care was improved. Then the ED leaders—Andrew Muck, MD, and Steven Moore, MD—turned to the hospital for relief from high boarding levels. Their message was simple and powerful: “We fixed our house. Now can you help us with boarding?”
On the heels of the success in the emergency department, hospital leadership responded to this request favorably. They set out to increase inpatient capacity by improving discharge by noon (DBN). Note that DBN is measured as the percent of discharged patients out of beds by noon, not merely those who have a discharge order. Most hospitals experience discharge delays because discharge processes have become complex, are poorly articulated, and are not well synchronized. Things that must happen before a patient goes home often occur in a random fashion, and task roles are unclear. This frequently results in patients leaving the hospital later in the day, long after the ED demand for inpatient beds has risen. This, above all, causes boarding.
Communication around discharge is also haphazard. Common barriers to early discharge include transportation, physical therapy, follow-up appointments, durable medical equipment, medications, and education. Coordinating all of these elements understandably proves challenging on the inpatient side.
Cooperation and Coordination
The improvement initiative at UHS (dubbed “Power Through!”) focused on the discharge process itself, with a goal of increasing DBN without increasing LOS. The team began in the fall of 2018 with a kickoff lecture by Katherine Hochman, MD, of New York University Medical Center in New York City, who has published her successful work. She was able to alleviate boarding by increasing early discharges from the inpatient hospitalist units. UHS asked each unit and service to address the process of discharge on their units, the communication around discharges, and tools necessary to facilitate that discharge (see Figure 1). A key element in Dr. Hochman’s work and the work at UHS was “discharge rounding”—the implementation of brief discharge-focused rounds that coordinate the discharge of a patient a day or two in advance of an anticipated discharge. Getting ahead of the discharge process and communicating about the discharge to all stakeholders were critical to the project’s success.

Figure 1: Key Elements of UHS’s Power Through! Plan
Rollout of this program included a retreat that helped to articulate unit level discharge processes, discharge communication, discharge rounds, and tools to support the work. Figure 2 is a sample swim lane diagram articulating the discharge process on a typical unit.
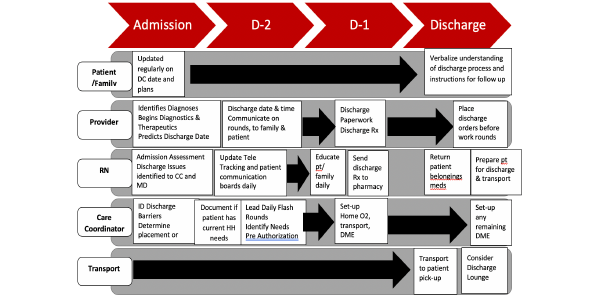
Figure 2: Sample Swim Lane Diagram of the Discharge Process
The Results
The hospital at-large and the adult services unit performed particularly well (see Figure 3). This project was driven by nursing leaders Nelson Tuazon, assistant chief nursing officer, and Missam Merchant, director of the central operations management group. Note the dramatic increase in early discharges.
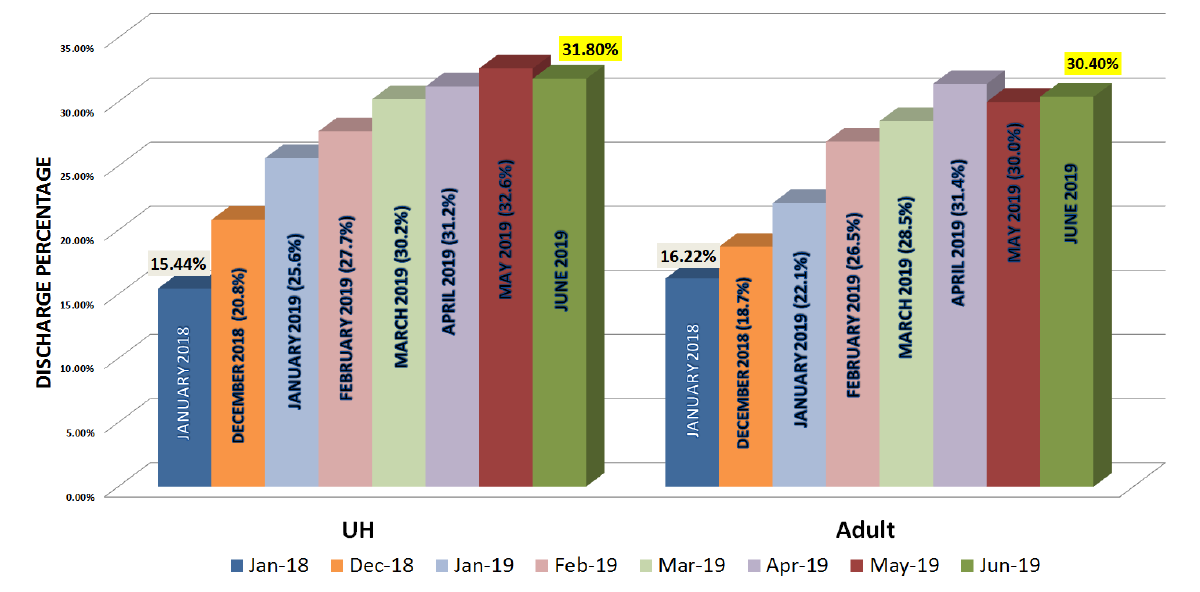
(click for larger image) Figure 3: Discharge Before Noon Trends for University Hospital and Its Adult Services Unit
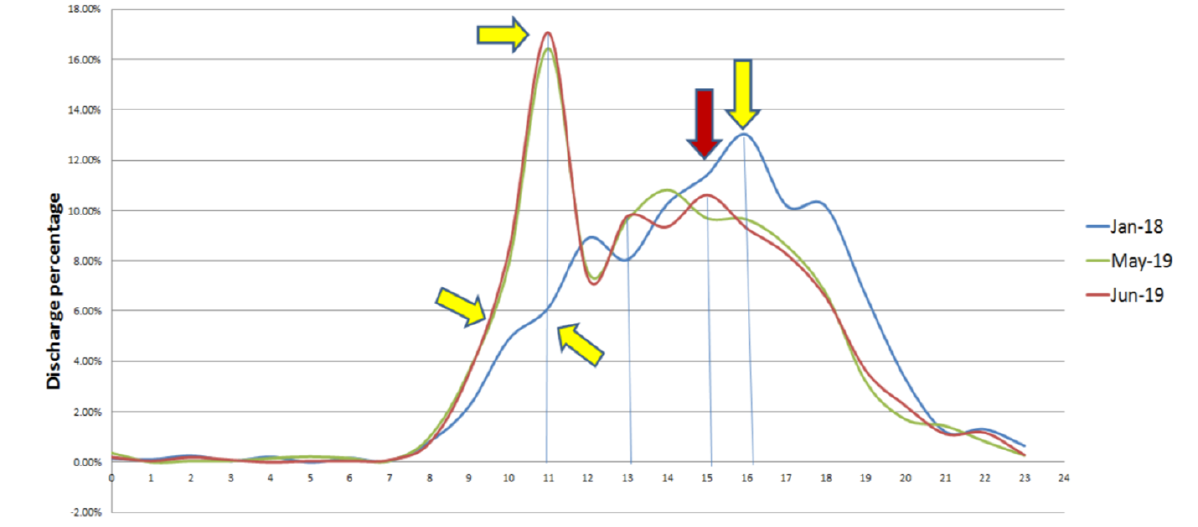
The effect of early inpatient discharge on ED boarding is impressive (see Figure 4). By initiating discharge momentum earlier, beds opened up for ED admissions, which begin late in the morning and continue throughout the day.
At UHS, boarding had been difficult to manage. The increased DBN project had an immediate effect. This nursing-led inpatient project had the support of the dean, the medical school chairs, and the hospital leaders. With everyone aligned with the mission, they recovered wasted capacity without spending a penny on new inpatient rooms. The hospital has improved on its boarding problem so effectively that the emergency department has consistently avoided diversion for the past six months.
The take-home message is there are boarding solutions out there if your hospital is willing to Power Through!
Pages: 1 2 | Multi-Page






No Responses to “How Did University Hospital in San Antonio Reduce ED Boarding?”