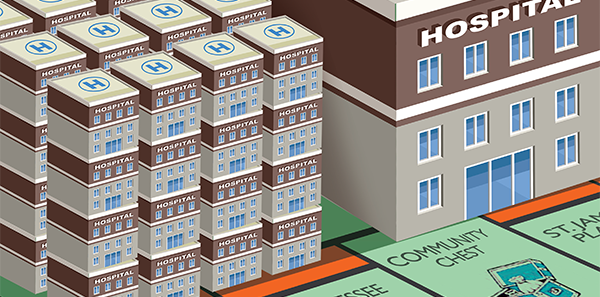
Consolidation in the health care market isn’t a new trend, but the frenzy of mergers and acquisitions in the emergency medicine space make this a top concern for practicing emergency physicians and EM administrators. Over the next few months, ACEP Now will feature a series of articles exploring the effects—both positive and negative—that consolidation may have on emergency medicine.
Explore This Issue
ACEP Now: Vol 34 – No 12 – December 2015To start the discussion, ACEP Now editorial board member Ricardo Martinez, MD, FACEP, chief medical officer for North Highland Worldwide Consulting and assistant professor of emergency medicine at Emory University in Atlanta, recently sat down with Jeff Swearingen, managing director and cofounder of Edgemont Capital Partners in New York City, to explore some of the forces driving mergers and acquisitions in emergency medicine. Next month, we’ll highlight some of the mergers and acquisitions topics discussed at the ACEP15 Council Town Hall meeting held Oct. 25, 2015, in Boston.
RM: We’re seeing a lot of activity and tremendous interest in mergers and acquisitions in emergency medicine. What do you see as the main driving forces behind this?
JS: First and foremost, there’s a lot of mergers and acquisitions activity throughout health care right now. There is consolidation happening in all four of the main hospital-based specialties: emergency medicine, anesthesia, hospitalist medicine, and radiology. Anesthesia is even more active than emergency medicine in terms of the number of transactions at the moment, if you can believe that. Consolidation is resulting from different types of provider organizations jockeying for position and negotiating leverage as people look to negotiate a larger share of a bundled payment that may be bundled across both the facility and the provider in the future. I think the second reason for consolidation is access to capital. Many of the consolidators that are driving mergers and acquisitions in emergency medicine have far greater access to both debt and equity capital than even a midsized regional group might have. Investment in information technology and other capabilities will be important going forward, especially the ability to capture data beyond just the three hours in the emergency room episode of care. Emergency physicians in the future may be able to capture data via call center follow-up with patients to make sure that they’re following their discharge instructions and that they’re making follow-up appointments with their office-based providers. Envision, the EmCare business, also owns the large ambulance company American Medical Response, and they are using the trained paramedics to make follow-up house calls to patients discharged from their EmCare-staffed emergency rooms. They’re doing this on a test basis in some markets, as I understand it. Envision is using those resources to try to reduce readmission cases. That is just one example of what may be required of emergency medicine providers in the future. To meet these potential requirements, groups will need expertise beyond emergency medicine, information technology resources, and access to capital to make those types of investments.
RM: What do you see as some of the biggest challenges for these organizations as they begin to merge different entities together?
JS: I’ll be the first to tell you, having worked on mergers and acquisitions for 20 years, that there’s absolutely a challenge to making mergers and acquisitions work. Many physicians, whether it’s in emergency medicine or any other specialty, are used to owning their own practice. If they merge with a large organization, it’s critical that the culture of hard work, high clinical standards, and feeling a sense of ownership and pride in their practice continues to be fostered and supported. We have seen mergers and acquisitions go quite well for several of the groups we’ve represented, but we’ve also seen where there were some stumbles. At the end of the day, both of those parties have to live up to the plan under which the transaction was entered into in order to make it work.
RM: We’ve watched the valuations and the multiples rise pretty quickly over the last few years. Do you see this as a temporary situation?
JS: I’ll say this: From a relative basis, valuations are higher now than they have been at any point in the last five years, maybe even the last 10 or more years. Part of that is driven by the fact that, for the most part, capital markets are doing very well right now. The large consolidators have access to plenty of debt and equity capital at a relatively low cost. Part of that is because of the scarcity value [the economic factor that increases an item’s relative price based more upon its relatively low supply] of some of the really high-quality groups. In the last year or two, we’ve seen several very large transactions in emergency medicine, like Premier Physician Services and Emergency Medical Associates of New Jersey. With those very large groups, there’s scarcity value. My general perspective is that if you’re a seller, valuations are very attractive right now.
RM: We’re seeing this move to consolidate in a lot of industries. Many of the benefits are back-office benefits: administrative benefits, billing and coding, tracking data, etc. As these types of services become more cloud-based, do you see some undoing of the need to consolidate?
JS: I certainly believe there’s always going to be a position and presence in the market for independent groups. That being said, what is going to be increasingly important for those groups to maintain their independence is the ability to access low-cost, high-quality back-office services and be able to access, via information technology, the quality metrics, the data analytics that they need to demonstrate their value in the marketplace. If independent groups are determined to stay independent, they absolutely need to be focused on how to best access those capabilities and services.
RM: In the next five years, where should emergency physicians be looking to maximize their role in the value chain that’s emerging?
JS: It comes back to the importance of being able to measure your impact on a patient’s health and affect outcomes beyond the episode within the four walls of the emergency room. That could be measured by increased data gathering and quality metrics within the acute episode of care in the emergency room as well as by the ability to reach that patient and the patient’s follow-up physicians to affect care as [the patients] return to their homes.
Pages: 1 2 3 | Multi-Page





No Responses to “How Health Care Consolidation Is Changing Emergency Medicine”