
COVID-19 has infected more than 247 million people worldwide, leading to over 5 million deaths.1 Distribution of critically ill patients to available critical care units and tertiary centers for specialized care has been an essential strategy to maximize health system resources. These circumstances have put a strain on and created unique needs for air medical transport in the United States.
Explore This Issue
ACEP Now: Vol 40 – No 12 – December 2021STAT MedEvac is a regional critical care transport network serving a catchment area of roughly 4 million people. Affiliated with the University of Pittsburgh Medical Center, STAT MedEvac transports 13,000 patients per year, operating 18 base sites serving five states and the District of Columbia. Since March 2020, we have developed and refined comprehensive procedures to address the clinical needs posed by the COVID-19 pandemic and, to date, have transported over 2,000 confirmed or suspected COVID-19 patients.
Clinician Safety and Personal Protective Equipment (PPE)
Early in the pandemic, managing uncertainty regarding transmission, diagnosis, prevention, and treatment called for definitive, dynamic procedures. For real-time education and communication, we implemented weekly systemwide video conferences to discuss current recommendations, answer questions, and facilitate necessary changes. Daily operations calls at shift change addressed more immediate needs.
To reduce on-duty exposure, we established a preshift health assessment. Staff who screened positive were referred to regional management and occupational health. We also enacted universal masking while on duty; instituted daily cleanings; and deployed physical distancing and barriers in our administrative offices, maintenance areas, and communications center.
A three-tiered system identified patient COVID-19 status prior to transport. First, our referral center screened for known infection. Once a transport asset was requested, our communications center performed a second-level screen with the referring facility including symptoms and testing for COVID-19. At bedside, crews performed a third, more thorough screening based on symptoms, lab studies, and clinical assessment to identify patients of interest (PUIs). In accordance with recommendations from the World Health Organization (WHO) and the Air Medical Physician Association (AMPA), personnel used airborne precautions for all PUIs.2

STAT crew at base, ready with PPE.
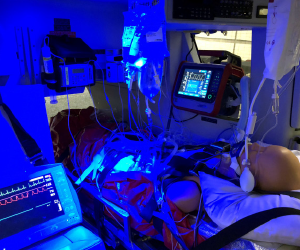
Typical setup inside STAT MedEvac aircraft, featuring a loaded patient on ventilator, multiple infusions, and balloon pump.
During the first wave of COVID-19, we employed a PPE strategy that included surgical masks for all patients and crew, escalating to eyewear, N95 mask, surgical gown, and gloves if the patient met COVID-19 high-risk criteria (including any of the following: positive or pending COVID-19 test, isolation status, close contacts within 21 days, fever absent alternate source, suspected respiratory infection, noninvasive or high-flow ventilation, or need for aerosolizing procedures). We had no known patient-to-staff case transmission during that time. However, the second wave brought an increasing number of COVID-positive patients missed by screening, including trauma and stroke patients from missions where limited history was available. To mitigate unexpected crewmember quarantines, in October 2020, we adjusted our requirements for crew to wear elevated levels of PPE for all patient interactions. To offset supply concerns, N95s were reused per Centers for Disease Control and Prevention recommendations. Additionally, each crewmember was issued a half-face respirator containing removable P100 filters that permitted easy disinfection. To ensure appropriate resource allocation, we tracked PPE stock counts daily at each base and communicated to central management.
Vehicle Logistics
The air medical transport environment (in Airbus EC-135 and EC-145 helicopters) presented a challenge to maintaining isolation precautions because patients and staff were contained in small compartments with unavoidable prolonged exposure (median flight time 19 minutes; interquartile range 13–31 minutes). Because only a cloth divider separates the cockpit and main cabin, even our pilots don N95 masks for all patient transports. To avoid unnecessary exposure, they remain in the cockpit, stay out of patient clinical areas, and do not assist in patient loading or unloading. In the aircraft cabin, outside air ventilation is selected over air recycling.
Following transport of COVID-19 patients or PUIs, aircraft and equipment undergo a regimented decontamination process. All equipment is removed from the aircraft, and the floor of the airframe, the stretcher, and equipment tracks are swept. The entire patient compartment and all equipment are then sprayed with disinfectant (3M’s TB Quat) and allowed to dry. After an appropriate dwell time (minimum 20 minutes), the main cabin is wiped down with antiseptic wipes before returning the equipment. Recently, we adopted the use of an AeroClave fogger for more efficient decontamination.
Pages: 1 2 3 | Single Page




No Responses to “How One Air Transport Network Adjusted to the COVID-19 Era”