A 50-year-old female develops chest pain radiating to the neck and left arm. ECG, CXR, and troponin are negative. She is given morphine for pain. Four hours later she develops back pain and bilateral leg paresthesias. CT angiography shows aortic dissection which is treated surgically, but she is left with paraplegia.
Explore This Issue
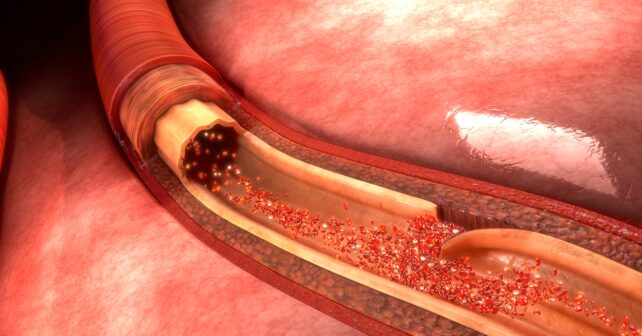
ACEP Now: Vol 42 – No 06 – June 2023Notoriously elusive, with a high misdiagnosis rate, thoracic aortic dissection (AD) can mimic many conditions, including acute coronary syndrome (ACS, the most common), gastroesophageal reflux disease (GERD), stroke, and spinal-cord compression.1 Opioids or anxiolytics are often given to patients whose diagnosis of AD is missed or delayed. The fact is that no benign thoracic disease such as non-ischemic ACS or GERD should require morphine or benzodiazepines.
The varied clinical presentations described below illustrate some of the many faces of AD.
Trap #1: Walks like a duck, quacks like a duck, but it’s not a duck. Then what?
1. A 42-year-old male develops sudden anterior chest pain radiating to his jaw while eating. He denies back pain. A medical student reports a murmur, not documented by either the emergency physician or the cardiologist. Troponins #1 and #2 are borderline and ECG is non-specific. The patient is admitted for ACS to a cardiologist who says he will see the patient in the morning. An echocardiogram the following morning shows 4+ aortic regurgitation and aortic dissection. The murmur is readily auscultated. The patient is treated surgically and survives.
2. A 35-year-old male develops sudden chest pain during an argument with his girlfriend over the phone. EMS is called and finds his blood pressure 175/100. He is given aspirin 162 mg and two doses of nitroglycerin, and his pain improves. On arrival his blood pressure is 126/90. In the ED, his troponin, ECG, and chest X-ray (CXR) are normal. He is given alprazolam for persistent symptoms and discharged. An aortic dissection is discovered when he bounces back to the ED. He survives.
Takeaway: AD does not have a classic presentation. In fact, 7 percent of ADs have none of the triad of acute tearing chest or back pain, mediastinal widening, or pulse or blood pressure differential. ACS is the most common misdiagnosis and often leads to inappropriate anticoagulation.1,2 Too often AD is missed due to anchoring or confirmation bias, where one assumes that the evidence supports one’s initial opinion. When the initial chest pain workup is complete, but the numbers don’t add up, broaden your differential. Listen to your gut. Morphine and benzos are rarely needed for stable ACS. Avoid looking for evidence to support your initial impression and instead start looking for evidence to prove yourself wrong.
Trap #2: Chest pain plus anxiety and neurological complaints. What if the anxiety is not the cause of the neuro symptoms?
1. A 55-year-old female with a history of GERD has rapid onset of epigastric pain, right hand numbness, blurry vision, and decreased sense of taste. ECG, CXR, and troponin are all normal. She is diagnosed with anxiety and given alprazolam, and dies eight hours later of aortic dissection.
2. A 38-year-old male feels a “pop” in his chest while lifting weights, followed a minute later by severe pain radiating into both legs. He arrives in the ED stating, “I can’t move my legs.” A consulting surgeon notes that he “is able to move his legs” and suspects malingering. He is given morphine and sent for a CT scan of the lumbar spine which reveals “multiple lumbar disc herniations.” While awaiting admission for “intractable back pain,” he dies of pericardial tamponade. A later review of the CT scan shows a visible abdominal aortic dissection flap that was missed.
Takeaway: Chest pain with neuro symptoms and anxiety can be the yellow brick road to disaster. Thoracic pain and any neurological complaint must include aortic dissection in the differential.
Any artery can be affected (e.g., a dissection can mimic lumbar disc herniation when it extends into the anterior spinal artery causing sudden paraplegia), which can wax and wane. Adding to the temptation to attribute the patient’s symptoms to anxiety, micro-emboli from a dissection’s turbulent flow can cause scattered, non-anatomic, sensorimotor symptoms, (e.g., loss of taste or tongue and hand numbness). And only a psychiatrist is allowed to use the word “malingering” in a medical record.
Trap #3: You’re too young to have an aortic dissection.
A 20-year-old male pushes a car up a hill when he notes sudden chest pain. An ECG and CXR are negative. He is given morphine for “costochondritis” and is discharged. He sees his primary doctor the next day, who schedules a stress test. The next day he collapses and dies. An autopsy shows a typical aortic dissection with tamponade and a bicuspid aortic valve.
Takeaway: Young people can have an aortic dissection, especially those with Marfan syndrome.
Trap #4: It’s been going on for days so you’re probably fine.
A 64-year-old smoker with hypertension develops chest pain and “pressure” in his neck. An ECG, CXR, and two troponins are normal. Symptoms improve with nitroglycerin and 1 mg of intravenous morphine. He is discharged and returns 4 days later with worse chest pain aggravated by breathing or moving. ECG, CXR, and troponins are again normal. He is again discharged and returns in another four days with chest pressure radiating to his right back and neck, left arm weakness, and shortness of breath. A third ECG and troponin are normal, but the CXR now shows the heart size to be at the “upper limits of normal.” A cervical CT is ordered and shows only degenerative joint disease. He is sent home a third time and dies of an aortic dissection four days later. The most recent CXR is reread and reported as showing a widened mediastinum.
Takeaway: Aortic dissection may progress slowly. The sooner it is diagnosed, the better. New onset chest pain requiring morphine should be a red flag.
Diagnostic Aids
Prediction Scores: The Aortic Dissection Detection Risk Score (ADD-RS) can reduce the chance of missing the diagnosis.3 It emphasizes three areas of focus:
- High-risk conditions (family history, aortic valve disease, Marfan’s, etc.)
- High-risk pain features (sudden onset, severity, quality)
- High-risk examination findings (pulse deficit, murmur, neurological deficit, etc.)
POCUS: Point-of-care ultrasound for AD is highly specific, but operator-dependent, and lacking in sensitivity—although late–model units can have sensitivity as high as 80-85 percent.4 It can be quick, if positive, and reduce time to surgery while awaiting a confirmatory CT angiography. Views of the carotids and the abdominal aorta if stroke symptoms or abdominal pain is present is an added benefit.
 Dr. Dajer was emergency department medical director at NY Presbyterian Lower Manhattan Hospital for 13 years.
Dr. Dajer was emergency department medical director at NY Presbyterian Lower Manhattan Hospital for 13 years.
 Dr. Pilcher is a retired emergency physician and ED medical director at EvergreenHealth in Kirkland, WA. He has served as a medical-legal consultant in malpractice cases throughout his career and is the editor/publisher of a free opt-in monthly newsletter “Medical Malpractice Insights – Learning from Lawsuits.”
Dr. Pilcher is a retired emergency physician and ED medical director at EvergreenHealth in Kirkland, WA. He has served as a medical-legal consultant in malpractice cases throughout his career and is the editor/publisher of a free opt-in monthly newsletter “Medical Malpractice Insights – Learning from Lawsuits.”
References
- Hansen MS, et al. Frequency of and inappropriate treatment of misdiagnosis of acute aortic Dissection. Am J of Cardiology. 2007;99(6):852-856.
- Von Kodolitsch Y, et al, Clinical predictors of acute aortic dissection. Arch of Int Med. 2000;160(19):2977-2982.
- Rogers AM, et al. Sensitivity of the aortic dissection detection risk score, a novel guideline-based tool for identification of AAD at initial presentation. Circulation. 2011;123:2213-18.
- Cecconi M, et al. The role of transthoracic echocardiography in the diagnosis and management of acute type A aortic syndrome. Am Heart J. 2012;163(1):112-18.
Pages: 1 2 3 | Multi-Page




No Responses to “How To Avoid Missing an Aortic Dissection”