Clinical hands-on training can be accomplished in the ED when learners are working alongside the USGNB champion. However, a busy ED shift can be suboptimal for teaching a new procedure, and learners can consider scheduling training shifts in the ED with the USGNB champion to perform blocks on acutely injured patients. The USGNB champion can also consider establishing agreements with the Anesthesia Department to allow learners to gain expertise from anesthesiologists performing USGNBs in the perioperative setting.
Explore This Issue
ACEP Now: Vol 42 – No 01 – January 2023Collaboration
An USGNB program requires buy-in from multiple hospital departments. Anesthesia, orthopedics, surgery, and other services may not be aware of the benefits of USGNBs for acute pain in the ED. We recommend formal meetings with various stakeholders to develop a clear interdepartmental plan for optimal pain control in patients with acute injuries. Using previously published data that defines benefits of ultrasound-guided femoral nerve blocks for hip fractures, we recommend service lines (emergency medicine, anesthesia, and orthopedics) build a vertical protocol (from the ED to the OR) that relies on a patient-centric approach to pain management. A collaborative, multidisciplinary, non-siloed care pathway provides patients with optimal care and leverages our anesthesia colleagues’ knowledge to teach the ultrasound-guided femoral nerve block to their more novice emergency medicine colleagues. This patient-centered approach to pain management can translate to other injuries that will be managed in conjunction with other service lines (e.g., rib fractures for the trauma service).5,6,7
First demonstrating USGNB proficiency on non-admitted ED patients (palmar lacerations, metacarpal fractures, rib fractures, etc.) will generate respect and trust from consultants. Prior to expanding USGNBs to patients whose care is multidisciplinary, it is essential to communicate and collaborate with everyone who will be caring for the patient downstream (orthopedics, trauma surgery, anesthesiology). Common concerns include documentation, masking of the neurologic exam or compartment syndrome, and peripheral nerve injury. While the body of literature supports the benefits and safety of USGNBs in the ED, these risks are rare, but real.
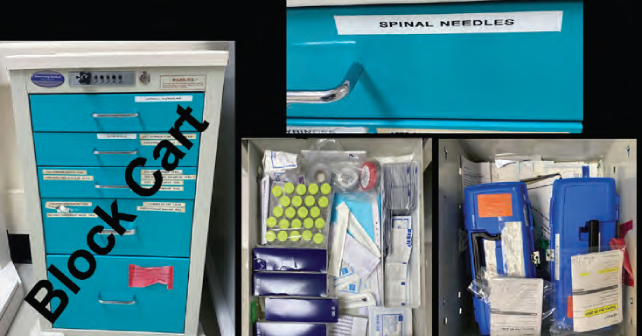
Having to rely upon nursing to retrieve medications can introduce barriers and time delays to executing USGNBs in your department. Protocols with pharmacy colleagues can provide access to local anesthetics, adjuvants, and intralipid outside of the Pyxis (or other automated medication dispensing systems) which can drastically improve clinician workflow. In our department, EPs bring a “block box” containing all of these medications to the bedside, place a patient sticker on the included inventory sheet and mark what medications were used, then return the block box to the ED pharmacist or charge nurse.



No Responses to “How To Build an Ultrasound-Guided Nerve Block Program”