Survey scan: Place a high-frequency linear transducer in the infraclavicular region with the cephalad portion of the probe resting on the medial portion of the clavicle (see Figure 3A). The transducer should be in parasagittal orientation with the probe marker facing cephalad. Slide the transducer laterally along the inferior portion of the clavicle (see Figure 3B). While sliding laterally, sonographically visualize the axillary artery in cross section as it emerges from under the clavicle (see Figure 3C), traverses the second rib, then courses away from the thoracic cage, appearing on ultrasound to be moving farther and farther from the clavicle. Fix the probe at the position where the axillary artery is 2–3 cm from the clavicle on the ultrasound (see Figure 3D). At this location, rotate the probe slightly to aim towards the axilla and identify the injection target, which lies just posterior to the artery.
Explore This Issue
ACEP Now: Vol 37 – No 10 – October 2018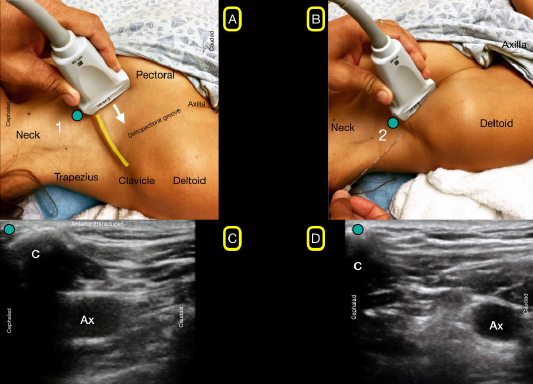
Figure 3A: The ultrasound probe is placed in the initial position (1) with the probe marker facing cephalad. 3B: Slide the ultrasound transducer along the inferior aspect of the clavicle until close to the deltopectoral groove (2). 3C: Note that in the initial position (1) the axillary artery (Ax) may be visible just under the clavicle (C). 3D: In the second position (2), the axillary artery (Ax) is visible and away from the pleura.
Credit: Luftig, Mantuani, Nagdev
Anesthetic: For a 70 kg patient, use 35–40 mL of 0.25% bupivacaine, 0.5% ropivacaine, or 1% lidocaine with epinephrine. Always adhere to weight-based local anesthetic dosing guidelines.
Needle type: Use a Tuohy 20g, 90 mm epidural needle (block needle) and a 25–27g hypodermic needle (for the local anesthetic skin wheal needle).
Injection setup: We commonly use a two-person technique to perform this block. One operator is advancing the needle under ultrasound visualization with the second operator slowly injecting the anesthetic while frequently aspirating to prevent inadvertent vascular puncture.
Injection: The primary challenge of the RAPTIR is passing the block needle through the “blind zone” created by the acoustic shadow of the clavicle during the initial portion of needle insertion. Keeping the transducer fixed over the injection target and aligned aiming towards the axilla, identify a block needle insertion site aligned with the long axis of the ultrasound beam and approximately 2 cm cephalad to the clavicle (see Figure 4A). This will ensure a safe needle path and allow adequate room for the needle to clear the posterior surface of the clavicle without angling posteriorly. Probing the insertion site with a gloved finger and seeing transmitted tissue motion on the ultrasound view help the operator get a feel for the needle insertion path and help determine if the insertion site is posterior enough to clear the clavicle.
Pages: 1 2 3 4 5 | Single Page




2 Responses to “How to Effectively Block an Acutely Fractured Distal Radius”
November 4, 2018
Mark BaileyNice if the ED MD can have a specialist come down. Too much time wasted for a real ED.
November 4, 2018
Michael Anthony MaciasLove this block and looking forward to incorporating into my practice though probably should reserve for more complex injuries as majority of distal radius fractures are easily reduced comfortably with a simple hematoma block.