Explore This Issue
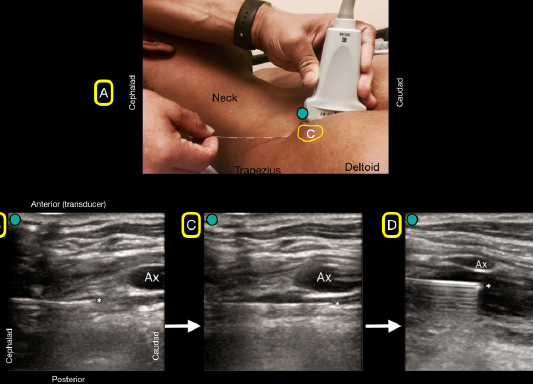
ACEP Now: Vol 37 – No 10 – October 2018Figure 4A: A flat needle angle will be used to traverse under the clavicle (C). 4B: The bock needle will have to pass under the clavicle and will not be visualized. Note the needle tip as it emerges from under the clavicle and can be easily seen because of its flat angle. 4C: The block needle is advanced until placed just under the axillary artery (Ax). 4D: Anechoic anesthetic fluid is injected under the axillary artery (Ax) for a successful block.
Credit: Luftig, Mantuani, Nagdev
Place a local anesthetic skin wheal at the insertion site using a 25–27g needle, then insert the block needle through the skin wheal and advance the needle beneath the clavicle toward the ultrasound beam at an angle parallel to the gurney (see Figure 4A). The patient should be prompted to alert the operator of any paresthesia in the shoulder while the needle advances, as the suprascapular nerve lies in the vicinity; this is a very uncommon occurrence. If the patient reports paresthesia of the shoulder, the needle should be withdrawn, and a slightly different needle path should be used. Also, when passing through the blind zone created by the clavicle, the needle should never be angled posteriorly, as this increases the risk of pneumothorax. However, the entire needle can be posteriorly deflected by applying pressure to the shaft at the insertion site while maintaining the same flat angle of approach, similar to the method used to get past the clavicle for a blind subclavian central line.
After insertion through the approximately 3 cm blind zone, use subtle needle and transducer adjustments to locate the clearly visualized needle emerging from beneath the clavicle (see Figure 4B). Continue advancing with in-plane ultrasound guidance toward the target location just posterior to the axillary artery, typically at or slightly past the six o’clock position relative to the artery (see Figure 4C). Aspirate to check for inadvertent vascular puncture and then inject small aliquots of normal saline. Anechoic anesthetic fluid should be seen spreading just posterior to the axillary artery and deflecting the artery toward the probe, confirming needle tip location within the axillary sheath (see Figure 4D). The sheath surrounds both the brachial plexus and the axillary artery. Thus, fluid injected into the sheath bathes the plexus. It is not necessary to visualize the nerves of the plexus. Once satisfied with the needle position, gradually inject local anesthetic until a total of 35–40 mL is deposited within the sheath. Total needling time is usually less than five minutes, and dense arm anesthesia develops within 30.
Pages: 1 2 3 4 5 | Single Page




2 Responses to “How to Effectively Block an Acutely Fractured Distal Radius”
November 4, 2018
Mark BaileyNice if the ED MD can have a specialist come down. Too much time wasted for a real ED.
November 4, 2018
Michael Anthony MaciasLove this block and looking forward to incorporating into my practice though probably should reserve for more complex injuries as majority of distal radius fractures are easily reduced comfortably with a simple hematoma block.