Imaging
Standard radiographs are indicated for both patellar and knee dislocations. In the case of patellar dislocation, pre-reduction radiographs may not be required at the discretion of the physician and based on confidence in diagnosis. Standard post-reduction radiographs of the knee should be obtained for both entities. For patellar dislocation, imaging is typically normal but may demonstrate avulsion fractures or loose bodies (see Figure 4).
Explore This Issue
ACEP Now: Vol 40 – No 03 – March 2021
Figure 4: X-ray of avulsion fractures/loose
bodies in patellar dislocation. Credit: John Kiel

Figure 5: X-ray of dislocated femorotibial
joint in a knee dislocation. Credit: John Kiel

Figure 6: X-ray showing
widened joint space. Credit: John Kiel
Point-of-care ultrasound can also rapidly evaluate the patellofemoral joint and extensor mechanism. Radiographs of a knee dislocation may show a clearly dislocated femorotibial joint (see Figure 5), which correlates to the physical exam.
In cases where spontaneous reduction occurred prior to arrival, radiographs can be normal. Other findings may show widened joint space (see Figure 6), fracture, or hemarthrosis.
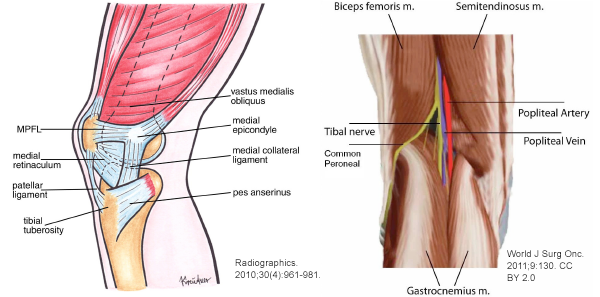
Consideration of vascular imaging is critical for all known or suspected knee dislocations. If there is evidence of an ischemic limb post-reduction, vascular surgery should be consulted for immediate transfer to the operating room. If the limb is well perfused but with an absent or asymmetrical pulse, CT angiography to assess for vascular injury is indicated. If the limb is well perfused and pulse is present, an Ankle Brachial Index (ABI) should be assessed. If the ABI is <0.9, CT angiography is indicated. If the ABI is ≥0.9, the patient should be admitted for 24-hour observation with serial vascular exams.17
Pre-reduction imaging of a knee dislocation is indicated in patients with good bilateral pulses to assess for concomitant fracture. If there is evidence of fracture, CT is recommended to further evaluate for preoperative planning.18
Rarely, this injury can occur in a patient following a total knee arthroplasty (TKA) (see Figure 7). This is most commonly seen in TKAs that retain the posterior cruciate ligament. Prevalence of this complication is low, at 0.15 to 0.5 percent.19 Reduction should occur in the operating room under general anesthesia, and in most cases, a complete surgical revision or an intercondylar constrained design is indicated.
Reduction and Disposition
In patients with patellar dislocation where spontaneous reduction has not occurred, the patella should be manually reduced. The analgesic approach is at the discretion of the physician; however, the reduction is often quick and easy to perform if the patient is willing, not requiring significant analgesia or procedural sedation. However, if it is anticipated that the patient’s level of pain or anxiety will make the reduction more difficult, a small amount of analgesia may be used.20 Simple reassurance, calming of the patient, and education on the reduction process are important. Here’s how to reduce a lateral patellar dislocation:20




No Responses to “How To Identify and Treat Patellar Dislocation Versus Knee Dislocation”