
A 77-year-old man presented to the emergency department (ED) with hip pain following a fall. On ED presentation, he was experiencing 10 out of 10 pain level. Physical examination was notable for left lower extremity with foreshortening and external rotation. A radiograph is shown (see figure 1).
Explore This Issue
ACEP Now: Vol 43 – No 02 – February 2024Problem
How should his pain be managed?
The risks of opioid medications, especially in the elderly, has been well described.1–4 Emergency physicians commonly prescribe opioid pain medications, and there is significant variability among prescribing patterns.5 A recent study found that 10 percent of opioid pain prescriptions are associated with indicators of inappropriate prescribing, and 42 percent may be misused or diverted.1 Alternatives to opioid pain management may include non-opioid systemic agents, such as acetaminophen, nonsteroidal anti-inflammatory agents, ketamine, steroids, or local or regional anesthesia.
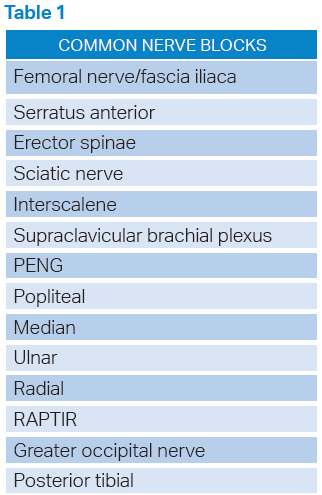
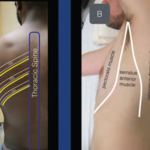
In the January issue of Annals of Emergency Medicine, Merz-Herrara, et al., published a study, “Safety and Pain Reduction in Emergency Practitioner Ultrasound-Guided Nerve Blocks: A One-Year Retrospective Study.”1 The authors describe a retrospective study of 420 patients who received ultrasound guided nerve blocks. Among 420 patients, only one patient experienced a complication, an arterial puncture which was recognized through syringe aspiration and without further sequelae). Of the 261 patients with preblock and postblock pain scores, there was significant improvement in postblock pain scores. The pain scores decreased from 7.4 (mean) to 2.8 (mean).
 Case Resolution
Case Resolution
This study reaffirms the safety and efficacy of ultrasound nerve blocks. This patient may benefit from an ultrasound guided femoral nerve block (fascia iliaca), which may eliminate or reduce the need for opioid medication and its potential adverse effects.
Dr. Marco is professor of emergency medicine at Penn State Health-Milton S. Hershey Medical Center in Hershey, PA, and associate editor of ACEP Now.
References
- Gharibo C, Drewes AM, Breve F, Rekatsina M, Narvaez Tamayo MA, Varrassi G, Paladini A. Iatrogenic Side Effects of Pain Therapies. Cureus. 2023 Sep 2;15(9):e44583.
- Herzig SJ, Anderson TS, Urman RD, Jung Y, Ngo LH, McCarthy EP. Risk Factors for Opioid-Related Adverse Drug Events Among Older Adults After Hospitalization for Major Orthopedic Procedures. J Patient Saf. 2023 Oct 1;19(6):379-385.
- Calcaterra SL, Yamashita TE, Min SJ, Keniston A, Frank JW, Binswanger IA. Opioid Prescribing at Hospital Discharge Contributes to Chronic Opioid Use. J Gen Intern Med. 2016 May;31(5):478-85.
- Kuo Y.-F., Raji M. A., Chen N.-W., Hasan H., Goodwin J. S. Trends in opioid prescriptions among part D medicare recipients from 2007 to 2012. American Journal of Medicine. 2016;129(2):221.e21–221.e30.
- Barnett ML, Olenski AR, Jena AB. Opioid-Prescribing Patterns of Emergency Physicians and Risk of Long-Term Use. N Engl J Med. 2017 Feb 16;376(7):663-673.
- Lyapustina T, Castillo R, Omaki E, Shields W, McDonald E, Rothman R, Gielen A. The Contribution of the Emergency Department To Opioid Pain Reliever Misuse And Diversion: A Critical Review. Pain Pract. 2017 Nov;17(8):1097-1104.
- Merz-Herrala J, Leu N, Anderson E, Lambeck A, Jefferson J, Sobrero M, Mantuani D, Mudda G, Nagdev A. Safety and Pain Reduction in Emergency Practitioner Ultrasound-Guided Nerve Blocks: A One-Year Retrospective Study. Ann Emerg Med. 2024 Jan;83(1):14-21.
Pages: 1 2 | Single Page





No Responses to “How to Manage Elderly Patient Pain without Opioids”