
The clinician should clearly visualize the fluid deposition on the ultrasound screen, and use this fluid to lift the nerve bundle away from the first rib (Figure 4). The clinician should then deposit small aliquots (3 to 5 cc max) every 15 to 30 seconds until the predetermined total anesthetic is deposited. If the needle location is adequate, a single injection should suffice, but repositioning the needle superiorly may be necessary to surround the nerve sheath completely with anesthetic. Once your injection is complete, gently remove the needle and dress the injection site as needed.
Explore This Issue
ACEP Now: Vol 42 – No 04 – April 2023Aftercare
Mark the affected extremity with the date, time, and type of block performed. Document the block in the electronic health record. Communicate with nurse(s), other providers, and any relevant consultants that a block was performed. Reassess the patient to ensure adequate analgesia and assess the efficacy of the block. Also, reassess and document a repeat neurovascular examination.

FIGURE 4A: Schematic representation of a block needle entering lateral to medial in-plane and depositing anesthetic between the brachial plexus and first rib. (Click to enlarge.)
Conclusion
For upper extremity injuries, traditionally procedural sedation, local anesthesia, and hematoma blocks have been used for pain management during procedures in the ED. However, these strategies have their own disadvantages such as increased resource allocation for procedural sedation and possibly incomplete analgesia for hematoma blocks depending on the location. Brachial plexus blocks such as the supraclavicular block provide adequate analgesia for a larger variety of upper arm injuries when compared to the hematoma block and require fewer resources when compared to procedural sedation. This nerve block is safe, easily learned, and does not require advanced ultrasound training to perform.11
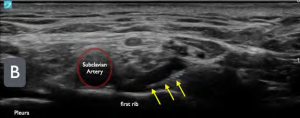
FIGURE 4B: Ultrasound image of a supraclavicular brachial plexus block. (yellow arrows = block needle). Note the anechoic (black) fluid between the first rib and the brachial plexus. (Click to enlarge.)
With an increase in the number of patients boarding in the ED, potentially decreased availability of procedural sedation rooms, and increasing patient-to-nurse ratios, ED physicians must adapt and become more efficient with limited resources. The supraclavicular block will not solve these systemic issues, but rather provides a more efficient strategy to manage pain better from acute upper extremity injuries as well as an alternative to procedural sedation in the ED.
Dr. Ayala is an emergency medicine resident at Highland General Hospital, Alameda Health System in Oakland, California.
Pages: 1 2 3 4 5 | Single Page





No Responses to “How To: The Ultrasound-Guided Supraclavicular Brachial Plexus Block”