
Explore This Issue
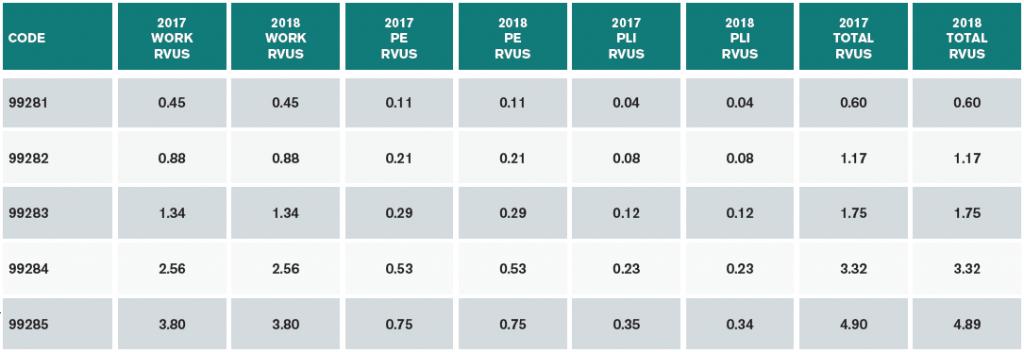
ACEP Now: Vol 37 – No 01 – January 2018(click for larger image) Table 1. 2018 Emergency Department E/M RVUs 99281–99285, 99291
RVU= relative value units; PE=practice expense; PLI=professional liability insurance
2018 CPT Changes for Emergency Medicine
There are two changes to the 2018 CPT book that are relevant to emergency medicine.
The first is subtle, with the two words “outpatient hospital” having been inserted into the preamble for the observation codes. The opening sentence now reads, “The following codes are used to report encounter(s) by the supervising physician or other qualified health care professional with the patient when designated as outpatient hospital ‘observation status’ [emphases added].” Similar language has also been inserted into the code descriptors.
Depending on the context, this leaves open to interpretation whether a hospital-based location is required for reporting observation services.
The second change pertains to new chest X-ray codes, which will describe the number of views ordered rather than describe what those views entail. Codes 71010–71022 have been deleted in 2018 and have been replaced with codes 71045–71048. The new codes describe a radiological examination; chest single view; and then two, three, and four or more views, respectively.
Merit-Based Incentive Payment System (MIPS)
MACRA has had many long-lasting effects. The hated Sustainable Growth Rate (SGR) formula, which mandated years of potential draconian double-digit provider reimbursement cuts, no longer impacts provider payments. However, CMS has moved forward a much more complex quality-reporting program. The prior programs of the Physician Quality Reporting System (PQRS), the Value-Based Modifier, and Meaningful Use have now been rolled up into the Merit-Based Incentive Payment System (MIPS). Under MIPS, providers will see reimbursement adjustments impacting 2020 payments based on 2018 reporting in four categories:
- Quality
- Resource use
- Improvement activities
Meaningful use of an electronic health record (EHR) system
For the 2018 performance year (impacting 2020 payments), the four MIPS categories will be simplified for most emergency physicians. The final rule assigned the resource use category a weighting of 10 percent for 2018 (likely increasing to 30 percent for 2019). In addition, if providers deliver more than 75 percent of their Medicare services in an emergency department, they are excused from the meaningful use of EHR component. The consolidated program is then reweighted in 2018 to 75 percent quality (the old PQRS program), 10 percent cost, and 15 percent improvement activities (see Table 2).
Pages: 1 2 3 | Single Page





No Responses to “Impact of 2018 CMS Physician Fee Schedule on Emergency Physicians”