The cost of out-of-network care has come under scrutiny and grabbed media attention as physicians, insurance companies, and legislators grapple with the issue of “surprise billing.” Emergency physicians have cited narrow networks and skimpy insurance coverage as the major reasons costs have been shifted to patients. Insurance companies, meanwhile, have promoted the narrative that emergency physicians intentionally stay out of network in order to charge higher prices.
Explore This Issue
ACEP Now: Vol 38 – No 07 – July 2019The insurance industry has been particularly critical of independent freestanding emergency departments (FSEDs), which have been a disruptor to the market in Texas. Some FSEDs exist as hybrid models, combining an emergency department with an urgent care facility to try to improve price transparency and reduce costs for lower-acuity visits. There are studies suggesting that FSEDs may decrease admissions, which may also reduce costs.1 It was presumed that insurance companies would want to contract with these facilities to save money. However, many owners were unable to get a contract (or even a return phone call) from most of the major health plans. This begs the question of whether physicians were really intentionally trying to stay out of network or whether the health plans simply refused to negotiate in good faith.
We administered a survey in 2017 to investigate the percentage of independent FSEDs that were in-network with insurance companies and identify barriers to securing contracts. The survey was sent by email to all independent FSEDs in Texas, and data were collected about in-network status for facility and physician fees, affiliated urgent care or hybrid model design, number of attempts to contract, and barriers to successful negotiations. The survey found that:
- 25 of 38 physician groups responded to the survey (66 percent), representing 102 different independent FSEDs in Texas.
- 80 percent of independent FSEDs were not in-network for either physician or facility fees.
- 64 percent of FSEDs said they had not been contacted by an insurance company or had been unable to get an insurance company to return phone calls about contracting.
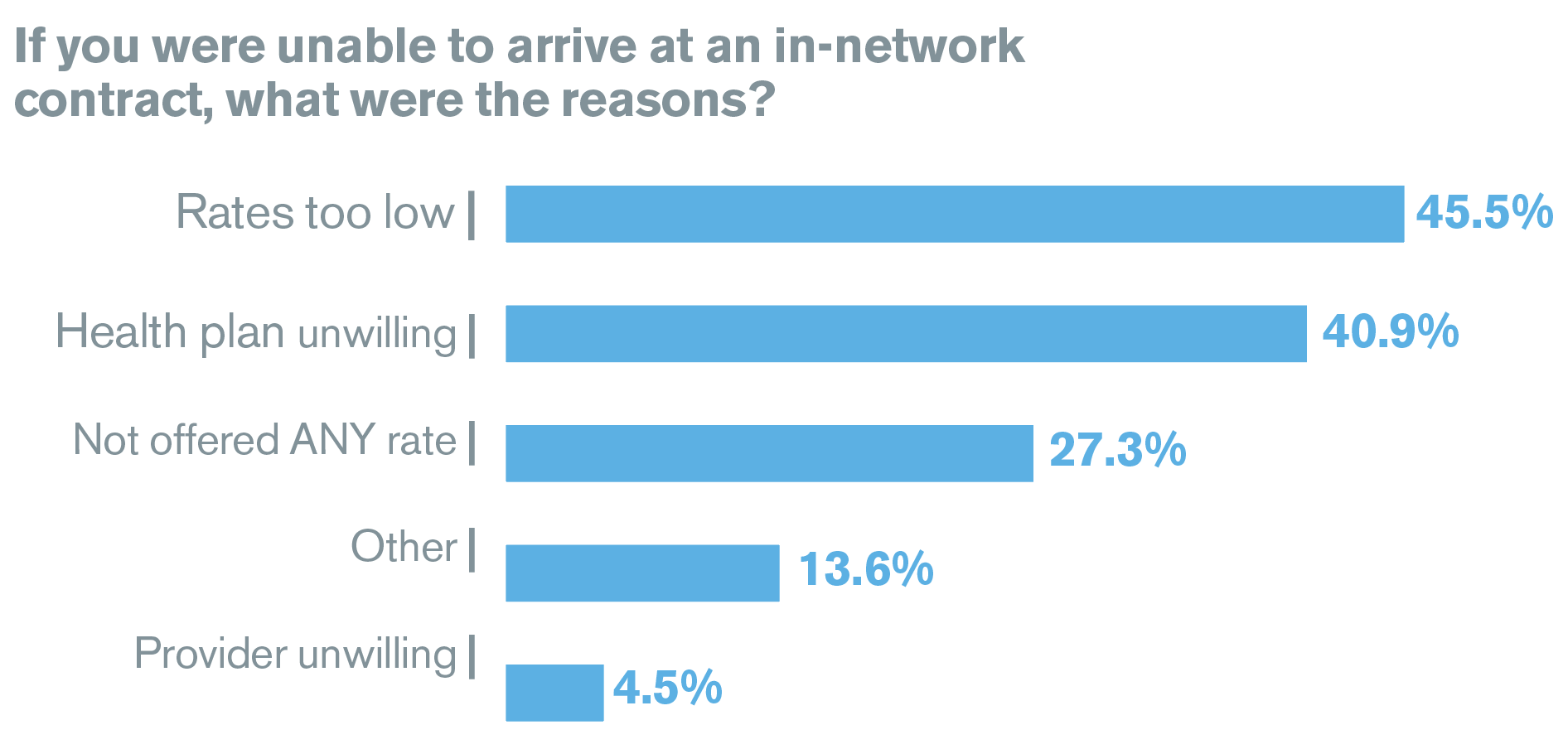
Failure to obtain in-network status occurred most frequently because rates were unreasonably low (45 percent), the insurance company refused to offer the FSED any contract (27 percent), and the insurance company did not want to contract with any FSEDs (41 percent). Physician groups did not want to contract with insurers only 5 percent of the time (see Figure 1).
Thus, despite a demonstrated desire of FSEDs to provide in-network care, only 20 percent were able to secure a contract with insurance companies.
The most common reason FSEDs were not in-network is that insurance companies did not offer to contract with them, ignored repeated attempts by physicians to negotiate, or offered unreasonably low rates and were unwilling to negotiate.
Although this study looked specifically at independent FSEDs in Texas, the concern is that insurance companies are using similar tactics nationwide. This is particularly challenging for small groups that have less leverage to negotiate, rural hospitals, and disproportionate share hospitals (ie, hospitals that see a high number of low-income patients and receive payments from the Centers for Medicaid and Medicare Services to cover the costs for uninsured patients), which have slimmer margins.
The health plans have a perverse incentive to avoid fair contracting because they know emergency departments are beholden to EMTALA and will take care of any patient, regardless of their ability to pay. Knowing that patients will be cared for regardless, insurance companies have little incentive to offer fair reimbursement rates.
Health plans need to be held accountable for offering reasonable in-network rates and providing adequate networks of care. Failure to do so results in decreased access and cost shifting to patients. Placing the blame on emergency providers only dirties the wound.
Reference
- Simon EL, Dark C, Kovacs M, et al. Variation in hospital admission rates between a tertiary care and two freestanding emergency departments. Am J Emerg Med. 2018;36(6):967-971.
 Dr. Simon is associate professor at the Northeast Ohio Medical University in Rootstown, research director for Cleveland Clinic Akron General emergency department in Akron, Ohio, and Medical Director of the Cleveland Clinic Bath emergency department.
Dr. Simon is associate professor at the Northeast Ohio Medical University in Rootstown, research director for Cleveland Clinic Akron General emergency department in Akron, Ohio, and Medical Director of the Cleveland Clinic Bath emergency department.
 Dr. de Moor is CEO of Code 3 Emergency Partners in Frisco, Texas, and chair and founder of Code 3 Emergency Physicians.
Dr. de Moor is CEO of Code 3 Emergency Partners in Frisco, Texas, and chair and founder of Code 3 Emergency Physicians.
 Dr. Dayton is adjunct assistant professor at the University of Utah in Salt Lake City, FSED Alpha Team for US Acute Care Solutions, and chair of ACEP’s Freestanding Emergency Centers Section.
Dr. Dayton is adjunct assistant professor at the University of Utah in Salt Lake City, FSED Alpha Team for US Acute Care Solutions, and chair of ACEP’s Freestanding Emergency Centers Section.
 Dr. Schmitz is associate professor at the F. Edward Hébert School of Medicine at the Uniformed Services University of the Health Sciences at San Antonio Military Medical Center.
Dr. Schmitz is associate professor at the F. Edward Hébert School of Medicine at the Uniformed Services University of the Health Sciences at San Antonio Military Medical Center.
Pages: 1 2 | Multi-Page





No Responses to “Insurance Companies Force Emergency Departments Out of Network, Shift Costs to Patients”