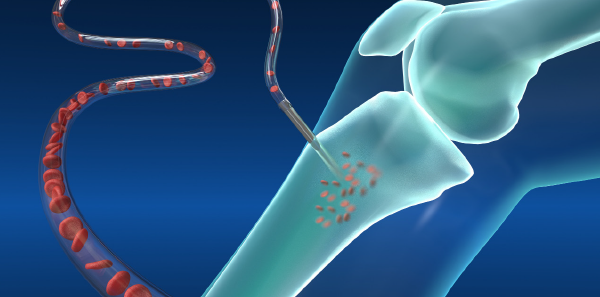
When you’re in an adult code and intravenous (IV) access can’t be obtained, the first option we reflexively go to is intraosseous (IO) access. Anyone who has practiced emergency medicine for more than a decade knows that was not always the case. In the 1980s, IO access was introduced as a standard of care by the American Heart Association as a component of pediatric advanced life support. During the decade or two that followed, IO access was mainly reserved for use in the pediatric population as an alternative to IV access. But in the early 2000s, its use in the adult population began to rise. The introduction of IO drills and use by the military helped increase adult use.
Explore This Issue
ACEP Now: Vol 40 – No 01 – January 2021First a little history: IO infusions were accidentally discovered in 1936 during experiments on bone marrow transplant in rabbits by Leandro Tocantins, MD, and John O’Neill, MD, in Philadelphia. When 5 mL of saline was injected into the proximal end of the bone, only 2 mL was recovered at the distal end, with no evidence of infiltration. Further studies were conducted using blood, and eventually a clinical trial was conducted using 14 human patients (including two children younger than 1 year old!), infusing blood, plasma, glucose, and saline. Initial injection sites used were the sternal body, manubrium, and distal femur or proximal tibia in infants. IO soon became a favored route for patients in shock, and it was also noted during the blitz of World War II that sternal puncture could even be carried out under poor light conditions.1
Despite the rise in its use and across nine decades of research, there are still many myths that persist regarding IO access.
Myth 1: The proximal tibia is the only location for insertion.
The proximal tibia is the most common site used, but there are multiple alternative locations an IO can be placed. Other locations include the distal tibia, proximal humerus, iliac crest, and sternum.
Myth 2: Only medications and crystalloid solutions can be infused through an IO.
As far back as the initial experiments with rabbits, IO access has been an option for more than just crystalloid fluids. Not only can any medication given intravenously be given through the IO route, but blood products and even IV contrast have been given successfully in some case reports.2,3 When paralytics for rapid sequence intubation were given via the IO route, first-pass success rate was 97 percent.4
Myth 3: IO infusions are too slow, and pressure bags can’t be used.
One concern is that because the IO is placed in the intermedullary space, flow rates need to be slower. But studies show flow rates of 4.96 mL/min in the proximal tibia and 2.07 mL/min in the distal tibia. Use of pressure bags increased the flow rate to 7.70 mL/min in the proximal group.5 These are still lower rates than a 14-gauge IV (366 mL/min) or triple lumen central venous catheters (CVCs) distal port (79 mL/min) but it provides a safe and effective path to the vascular system.6
Myth 4: IO access is hard to obtain.
In a study looking at out-of-hospital cardiac arrest, first-attempt success was more likely in the tibial IO group (91 percent) compared to the humeral (51 percent) or peripheral (43 percent) IV group. In a setting where medication delivery speed matters, it was also quicker to place the tibial IO (4.6 minutes) when compared to IV group (5.8 minutes).7 Success rates were also higher and achieved more quickly for IO when compared to CVC (85 versus 60 percent; 2 versus 8 minutes).8
Myth 5: There are no complications to placement of an IO.
All the above is true, but a procedure is a procedure. Though quick and easy to place, complications can occur. The most common complication is extravasation from a misplaced IO line. This can lead to compartment syndrome or tissue necrosis. Inappropriate placement can also lead to placement in the joint and not the intermedullary space.2 An IO line should never be placed in a limb that is fractured or has a vascular injury. If overlying cellulitis is present, or if previous orthopedic surgery has occurred in the location, IO placement may be unwise unless other options have been completely exhausted and the patient is crashing. A study performed in 1985 found the frequently reported serious adverse event was osteomyelitis (0.6 percent). All of these events occurred after prolonged IO infusions, suggesting that, once time permits, better intravascular access should be obtained.9
Myth 6: IO doesn’t hurt.
Awake patients do report pain, especially with infusions that create increased pressure in the intermedullary space. Recommendations for the awake patient include infusing lidocaine 2% (preservative free) over 120 seconds followed by allowing 60 seconds for the anesthetic to dwell in the IO space. In adults, the typical dose is 40 mg, and the pediatric dose is 0.5 mg/kg (maximum of 40 mg).10
Hopefully, this dispels any myths surrounding IO access and safe use. Next time you need to rapidly give medications and no IV access can be obtained, when appropriate, reach for the IO needle and drill.
 Dr. Sampson is director of education, director of clinical research, and assistant medical director of MU Emergency Medical Services and associate clinical professor in the department of emergency medicine at the University of Missouri–Columbia.
Dr. Sampson is director of education, director of clinical research, and assistant medical director of MU Emergency Medical Services and associate clinical professor in the department of emergency medicine at the University of Missouri–Columbia.
References
- Foëx BA. Discovery of the intraosseous route for fluid administration. J Accid Emerg Med. 2000;17(2):136-137.
- Rosenberg H, Cheung WJ. Intraosseous access. CMAJ. 2013;185(5):E238.
- Schindler P, Helfen A, Wildgruber M, et al. Intraosseous contrast administration for emergency computed tomography: a case-control study. PLoS One. 2019;14(5):e0217629.
- Barnard EBG, Moy RJ, Kehoe AD, et al. Rapid sequence induction of anaesthesia via the intraosseous route: a prospective observational study. Emerg Med J. 2015;32(6):449-452.
- Tan BKK, Chong S, Koh ZX, et al. EZ-IO in the ED: an observational, prospective study comparing flow rates with proximal and distal tibia intraosseous access in adults. Am J Emerg Med. 2012;30(8):1602-1606.
- Reddick AD, Ronald J, Morrison WG. Intravenous fluid resuscitation: was Poiseuille right? Emerg Med J. 2011;28(3):201-202.
- Reades R, Studnek JR, Vandeventer S, et al. Intraosseous versus intravenous vascular access during out-of-hospital cardiac arrest: a randomized controlled trial. Ann Emerg Med. 2011;58(6):509-516.
- Leidel BA, Kirchhoff C, Bogner V, et al. Comparison of intraosseous versus central venous vascular access in adults under resuscitation in the emergency department with inaccessible peripheral veins. Resuscitation. 2012;83(1):40-45.
- Rosetti VA, Thompson BM, Miller J, et al. Intraosseous infusion: an alternative route of pediatric intravascular access. Ann Emerg Med. 1985;14(9):885-888.
- EZ-IO intraosseus vascular access. Teleflex website. Accessed Dec. 11, 2020.
Pages: 1 2 | Multi-Page



2 Responses to “Intraosseous Myths: What ED Docs Should Know About this IV Alternative”
February 7, 2021
David A. Miramontes MD FACEP FAEMSYou forgot to mention the BEST IO site. THE DISTAL FEMUR in adults and peds. Better flow rates and can do cut down for obese patients with Yellow needle.
Though NOT “FDA approved” we use it extensively in EMS at San Antonio Fire Department and even infuse Whole Blood with no problem.
February 26, 2021
Stephen HoffmanThis IO article was very good. (My mentor at SF General Hospital was the doc who reincarnated the IO in the U.S., and pediatric EM in general, back in the ’80s.)
One caveat, though, about meds that can be used by the IO route: I agree that virtually everything CAN be used, but, from personal experience, I can tell you one drug that doesn’t work via IO. My patient was a 4-day old, who was brought in for fussiness and poor feeding. He had a regular and fixed HR of almost 300, narrow-complex. Dx: SVT. His color, sat., tone and CR were good, so we had time. We in the ED could not get in an IV, and after nearly 90 minutes, we finally put in an IO, in order to give adenosine. It did not work after multiple tries. The reason became obvious after thinking about it: the action of adenosine depends on getting the highest possible “instantaneous” concentration of the drug into the AV node, at one moment in time. This is why IV location (high up) and timing of the push and follow-up saline push are so important to success.
When this became obvious to us, we finally got smart and called up to the NICU, to ask a nurse to come down to the ED and help us start an IV. She did, got an IV in minutes, and we repeated the original dose of adenosine, but this time IV. Within seconds, the child was cardioverted to NSR, did very well, and went up to NICU for observation.
The take-home lesson was that whereas virtually every other drug, fluid, or blood product can be given IO, in the case of adenosine, (which has a unique mode of action, and depends on the highest possible “instantaneous” level of the drug in the AV node), you cannot achieve that peak level with the kinetics of adsorption from the marrow space into the circulation (IO route).
— Stephen Hoffman, MD