Case Resolution
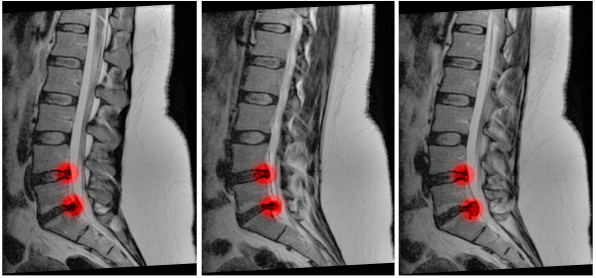
Your exam demonstrates decreased perineal sensation and weakness in L5 bilaterally. When questioned, the patient also highlights changes in bowel function. The patient’s PVR is 400 mL, and you call the surgeon, who asks for an MRI. The MRI demonstrates central disc protrusion at L5/S1. The patient is admitted and taken to the operating room.
Explore This Issue
ACEP Now: Vol 39 – No 02 – February 2020Dr. Long is an emergency physician in the San Antonio Uniformed Services Health Education Consortium at Fort Sam Houston, Texas.
Dr. Koyfman (@EMHighAK) is assistant professor of emergency medicine at UT Southwestern Medical Center and an attending physician at Parkland Memorial Hospital in Dallas.
References
- Tarulli AW. Disorders of the cauda equina. Continuum (Minneap Minn). 2015;21(1 Spinal Cord Disorders):146-158.
- Gardner A, Gardner E, Morley T. Cauda equina syndrome: a review of the current clinical and medico-legal position. Eur Spine J. 2011;20(5):690-697.
- Mauffrey C, Randhawa K, Lewis C, et al. Cauda equina syndrome: an anatomically driven review. Br J Hosp Med (Lond). 2008;69(6):344-347.
- Greenhalgh S, Finucane L, Mercer C, et al. Assessment and management of cauda equina syndrome. Musculoskelet Sci Pract. 2018;37:69-74.
- Moore KL. Clinically oriented anatomy. Baltimore: Williams & Wilkins; 1992.
- McNamee J, Flynn P, O’Leary S, et al. Imaging in cauda equina syndrome—a pictorial review. Ulster Med J. 2013;82(2):100-108.
- Fraser S, Roberts L, Murphy E. Cauda equina syndrome: a literature review of its definition and clinical presentation. Arch Phys Med Rehabil. 2009;90(11):1964-1968.
- Kapetanakis S, Chaniotakis C, Kazakos C, et al. Cauda equina syndrome due to lumbar disc herniation: a review of literature. Folia Med (Plovdiv). 2017;59(4):377-386.
- Kavanagh M, Walker J. Assessing and managing patients with cauda equina syndrome. Br J Nurs. 2013;22(3):134-137.
- Small SA, Perron AD, Brady WJ. Orthopedic pitfalls: cauda equina syndrome. Am J Emerg Med. 2005;23(2):159-163.
- Kostuik JP. Medicolegal consequences of cauda equina syndrome: an overview. Neurosurg Focus. 2004;16(6):e8.
- Markham DE. Cauda equina syndrome: diagnosis, delay and litigation risk. Curr Orthop. 2004;18(1):58-62.
- Fuso FA, Dias AL, Letaif OB, et al. Epidemiological study of cauda equina syndrome. Acta Ortop Bras. 2013;21(3):159-162.
- Korse NS, Pijpers JA, van Zwet E, et al. Cauda equina syndrome: presentation, outcome, and predictors with focus on micturition, defecation, and sexual dysfunction. Eur Spine J. 2017;26(3):894-904.
- Fairbank J, Hashimoto R, Dailey A, et al. Does patient history and physical examination predict MRI proven cauda equina syndrome? Evid Based SpineCare J. 2011;2(4):27-33.
- Domen PM, Hofman PA, van Santbrink H, et al. Predictive value of clinical characteristics in patients with suspected cauda equina syndrome. Eur J Neurol. 2009;16(3):416-419.
- Dionne N, Adefolarin A, Kunzelman D, et al. What is the diagnostic accuracy of red flags related to cauda equina syndrome (CES), when compared to magnetic resonance imaging (MRI)? A systematic review. Musculoskelet Sci Pract. 2019;42:125-133.
- Gleave JR, Macfarlane R. Cauda equina syndrome: what is the relationship between timing of surgery and outcome? Br J Neurosurg. 2002;16(4):325-328.
- Greenhalgh S, Truman C, Webster V, et al. Development of a toolkit for early identification of cauda equina syndrome. Prim Health Care Res Dev. 2016;17:559-567.
- Pronin S, Hoeritzauer I, Statham PF, et al. Are we neglecting sexual function assessment in suspected cauda equina syndrome? Surgeon. 2019. pii: S1479-666X(19)30037-X.
- Todd NV, Dickson RA. Standards of care in cauda equina syndrome. Br J Neurosurg. 2016;30(5):518-522.
- Gooding BW, Higgins MA, Calthorpe DA. Does rectal examination have any value in the diagnosis of cauda equina syndrome? Br J Neurosurg. 2013;27(2):156-159.
- Sherlock KE, Turner W, Elsayed S, et al. The evaluation of digital rectal examination for assessment of anal tone in suspected cauda equina syndrome. Spine (Phila Pa 1976). 2015;40(15):1213-1218.
- Todd NV. Guidelines for cauda equina syndrome. Red flags and white flags. Systematic review and implications for triage. Br J Neurosurg. 2017;31(3):336-339.
- Mukherjee S, Thakur B, Crocker M. Cauda equina syndrome: a clinical review for the frontline clinician. Br J Hosp Med (Lond). 2013;74(8):460-464.
- Goodman BP. Disorders of the cauda equina. Continuum (Minneap Minn). 2018;24(2, Spinal Cord Disorders):584-602.
- Kim JH, van Rijn RM, van Tulder MW, et al. Diagnostic accuracy of diagnostic imaging for lumbar disc herniation in adults with low back pain or sciatica is unknown; a systematic review. Chiropr Man Therap. 2018;26:37.
- Ozdoba C, Gralla J, Rieke A, et al. Myelography in the age of MRI: why we do it, and how we do it. Radiol Res Pract. 2011;2011:329017.
- Peacock JG, Timpone VM. Doing more with less: diagnostic accuracy of CT in suspected cauda equina syndrome. AJNR Am J Neuroradiol. 2017;38(2):391-397.
- Chau AM, Xu LL, Pelzer NR, et al. Timing of surgical intervention in cauda equina syndrome: a systematic critical review. World Neurosurg. 2014;81(3-4):640-650.
- Shapiro S. Medical realities of cauda equina syndrome secondary to lumbar disc herniation. Spine (Phila Pa 1976). 2000;25(3):348-351; discussion 352.
- Ahn UM, Ahn NU, Buchowski JM, et al. Cauda equina syndrome secondary to lumbar disc herniation: a meta-analysis of surgical outcomes. Spine (Phila Pa 1976). 2000;25(12):1515-1522.
- Aly TA, Aboramadan MO. Efficacy of delayed decompression of lumbar disk herniation causing cauda equina syndrome. Orthopedics. 2014;37(2):e153-156.
- Thakur JD, Storey C, Kalakoti P, et al. Early intervention in cauda equina syndrome associated with better outcomes: a myth or reality? Insights from the Nationwide Inpatient Sample database (2005–2011). Spine J. 2017;17(10):1435-1448.
Pages: 1 2 3 4 | Single Page




3 Responses to “Learn to Spot and Treat Cauda Equina Syndrome”
March 1, 2020
Jerry W. Jones, MD FACEP FAAEMExcellent review! Thank you!
March 1, 2020
Steven ShroyerNice analysis of diagnosing CES Brit and Alex. I was surprised at how poor each of the likelihood ratios are for this. Urinary retention appears to be nearly worthless. I see a fair number of patients with what I am calling “partial CES” and I frame it that way when speaking to the neurosurgeon because once it’s complete I assume it is permanent. This is usually in the pt who has back pain, bilateral paresthesias (or pain), has fallen but is not paralyzed and has had difficulty emptying their bladder. When combined this way maybe it has a higher +LR? In every case when I describe it as a “partial CES” to the surgeon they have performed decompressive laminectomy. Nice table of statistical characteristics. Thanks for the valuable information.
Steve Shroyer
March 1, 2020
CA Kennedy MFExcellent summary. Thanks!