Explore This Issue
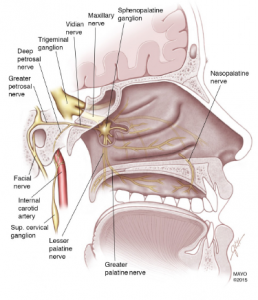
ACEP Now: Vol 37 – No 05 – May 2018Figure 1: The SPG is associated with the trigeminal nerve, the major nerve involved in headache disorders. It is an extracranial parasympathetic ganglion located behind the nasal bony structures. It has two ganglia, one in each of the bilateral fossae located posterior to the middle turbinate. It is made up of three nerves, the sensory, sympathetic, and parasympathetic.
Illustration: Headache. 2016;56:240-258.
The sphenopalatine ganglion (SPG) is associated with the trigeminal nerve, the major nerve involved in headache (HA) disorders (see Figure 1).1 The mechanism behind migraines is not fully understood, but it’s thought that blocking the SPG may help relieve migraine pain.1,2
The SPG is the main source of cranial and facial parasympathetic innervation. The autonomic nerves of the SPG supply the lacrimal glands, which produce tears, as well as the sinuses, which can produce the nasal discharge or congestion associated with some migraines.2-4
SPG’s Role in Headaches
When a headache occurs, meninges inflammation activates pain receptors. These receptors send pain impulses through the trigeminal nerve, which then sends a signal to the brain that is perceived as pain. In cluster and migraine HA, pain signals pass through the SPG, connecting with autonomic nerves, which produce eye tearing or nasal discharge. This is called the trigeminal autonomic reflex.3,4
During a migraine, parasympathetic outflow from the SPG causes vasodilation of cranial blood vessels. This dilation allows for inflammatory mediators to activate meningeal nociceptors, which are responsible for the migraine pain. It’s theorized that a patient who experiences parasympathetic symptoms during migraines (eg, nausea, emesis, sweating, lacrimation, etc.) may benefit from SPG blocking because the SPG propagates these parasympathetic signals.3,4
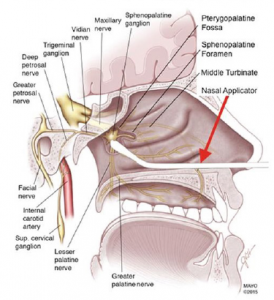
Figure 2: The cotton-tip applicator should contact the mucosa overlying the SPG.
Illustration: Anesthesiology. 2018;128(1):140.
A prospective, randomized and double-blinded placebo-controlled study published in JAMA in 1996 showed potential benefit for using intranasal lidocaine when compared with saline alone.5 The study included a total of 81 patients with a chief complaint of headache who fulfilled criteria for International Headache Society. The primary outcome measure found at least a 50 percent reduction of headache within 15 minutes of treatment. Fifty-five percent of patients had at least a 50 percent reduction of headache compared with 21 percent of patients in the control group, and nausea and photophobia were significantly reduced. Rescue medication for headache relief was needed in 28 percent of patients in the lidocaine group versus 71 percent of patients in the control group. Of those patients who showed initial improvement, only 42 percent relapsed versus 83 percent in the control group.
How to Perform an SPG Nerve Block
The SPG can be locally accessed by several approaches, but for the purposes of quick and easy access in the ED setting, the transnasal approach is best.3 The materials needed include:
- Cotton-tip applicator, 10 cm long
- Anesthetic of your choice:
- Lidocaine 1%, 2%, or 4% (onset 15 minutes, duration of action 30 minutes to 2 hours)6
- Bupivacaine 0.25% or 0.5% (onset 10–20 minutes, duration of action 2–4 hours)6
- 5 mL syringe and large bore needle to draw up the anesthetic
- Plastic pill cup or any small container that can hold the anesthetic with enough depth to fully submerge the cotton-tip applicator
- Atomizer (optional).
The technique:
- Have the patient lie in a supine position with the head tilted up in a sniffing position.
- Make sure the patient is on a cardiac monitor. Even though you are using less than the toxic dose, you are administering anesthetic over a highly vascular area.
- Anesthetize the nasal passage entry by one of two ways (optional):
- Inject 0.5 mL of 2% viscous lidocaine into each nostril with the open end of a 3 mL syringe (without needle). Have the patient sniff to draw the anesthetic posteriorly.
- Use an atomizer to draw up 1 mL of 1% lidocaine per naris and aerosolize into each naris. Remember, you can administer a maximum of 1 mL per naris.
- Soak one or two cotton-tip applicators in the anesthetic of your choice. If you are pre-anesthetizing the nasal passage, we recommend using only 1% or 2% lidocaine to soak the applicators, the goal being to remain well below the toxic dose.
- Advance one cotton-tip applicator along the superior border of the middle turbinate of each nostril until the tip contacts the mucosa overlying the SPG (see Figure 2).
- Leave the applicators in for 10 minutes or until the patient feels relief, then gently remove the applicators.3,7
Make sure you inform patients of the possible side effects so they know what to expect, including:
- Bitter taste from the anesthetic
- Nausea
- Local trauma causing epistaxis
- Light-headedness
- Numbness in the posterior pharynx4
Final Points
SPG nerve blocks are a quick and non-invasive way to treat primary headaches that do not require IV placement. Such blocks may be a good option for patients who feature difficult IV access.3
SPG blocks work best on headaches that have parasympathetic-related symptoms associated with them. SPG blocks can also treat temporomandibular joint disorders, trigeminal neuralgia, and post-herpetic neuralgia.
Finally, remember that epistaxis is an unlikely but potential complication.
Dr. Viguri is associate director of ED pain management at St. Joseph‘s Hospital in Paterson, New Jersey.
Dr. Paez Perez is an emergency medicine resident at St. Joseph’s Regional Medical Center.
References
- Schaffer JT, Hunter BR, Ball KM, et al. Noninvasive sphenopalatine ganglion block for acute headache in the emergency department: a randomized placebo-controlled trial. Ann Emerg Med. 2015;65(5):503-510.
- Jion Y, Robbins MS. The sphenopalatine ganglion (SPG) and headache. American Migraine Foundation website. Nov. 15, 2016. Accessed April 23, 2018.
- Shih J, Gaafary C. Trick of the trade: sphenopalatine ganglion block for treatment of primary headaches. Academic Life in Emergency Medicine website. March 22, 2017. Accessed April 23, 2018.
- Spector K, Sahai-Srivastava S. A new look at sphenopalatine ganglion blocks for chronic migraine. Practical Pain Management website. Aug, 7, 2017. Accessed April 23, 2018.
- Maizels M, Scott B, Cohen W, et al. Intranasal lidocaine for treatment of migraine: a randomized, double-blind, controlled trial. JAMA. 1996;276(4):319-321.
- Gadsden J. Local anesthetics: clinical pharmacology and rational selection. New York School of Regional Anesthesia website. Accessed April 23, 2018.
- Waldman S. Pain Review. Philadelphia, PA: Elsevier; 2009.
Pages: 1 2 | Multi-Page




21 Responses to “Migraine Care: Why and How to Block the Sphenopalatine Ganglion Nerve”
June 1, 2018
Jack Bragan MDDoes anyone routinely do this procedure ? and if so, is it difficult to get these patients to agree to this procedure ? and how good are your results ?
Thanks
June 14, 2018
Veronica B MDI’m a part of an online ED physicians group. I personally have not tried this, but other physicians are reporting good success. Sounds like they haven’t had problems getting patients to agree.
August 9, 2018
Adelaide Viguri, DOWe do routinely offer this block as part of our treatment for migraine and orofacial pain. I would say about a quarter of patients agree to the procedure, largely because it sounds more uncomfortable than it actually is. Patients that I performed the procedure on did not report any discomfort. I tried it on myself – the sensation of a cotton tip applicator in the tour nasal cavity does feels odd but otherwise, very tolerable. In my experience, I’ve had good results for migraines with autonomic symptoms and trigeminal neuralgia, but not successful for TMJ pain.
February 27, 2020
Barbie LongHi Doctor.
Do you know if these are effective for left sided moving into the facial and global?
June 14, 2018
Diana TowleMy daughter just had an SPG block with a doctor who uses the Sphenocath. She has been suffering from a constant 24/7 migraine for a year. The block eliminated her facial pain and pressure temporarily. It came back and made her realize how much facial pain and pressure she actually has which is good information to know as we are consulting with an ENT – though the pain in her temples is worse. She is having it done again as it seems the effects can be cumulative in chronic migraine patients. The hope is that it will calm and reset the nerve. It is one of the least invasive things a migraine patient can try.
September 10, 2018
Denise KI have had multiple SPG blocks and each has given me tremendous relief when oral medications (triptans, opioids, muscle relaxants,) and various IV medications in the ER failed. I have suffered from both migraines and TMJ disorder (bilaterally) for nearly 25 years. Sometimes the headaches are a mix of both, sometimes clearly one or the other. I did not hesitate when the SPG block was offered. The Q-tip type applicator was only tried once and it couldn’t be advanced far enough. So all of my blocks have been via a syringe with a really long needle or the SphenoCath device. No difference in either, just excellent and much-needed complete relief. Any discomfort is minimal and resolves quickly, or I wouldn’t have repeated this so many times.
August 29, 2019
Lisa KernDenise,
Have you been to an ENT to look at you septum? If it deviates to the side of the nose and touches, it could cause a migraine. A 20 minute in office surgery can fix it and it does have a strong correlation to migraines.
February 27, 2020
Barbie LongDo they let you have a supply of these at home?
September 17, 2018
Jan M.I have had the SPG procedure several times (I also have occipital nerve blocks in the back of my head same day). SPGs have been a great relief to what was debilitating pain behind and above my eyes after a brain injury. It is similar to a small catheter inserted momentarily in your nostril to pour the “magic medicine” down. It is within minutes, sometimes immediate, you feel relief. Very worth any initial awkwardness of having something put in your nose. Its quick and easy and provides great results!
October 29, 2018
Kimberly, RN, BSNWe started using the SphenoCath to deliver the anesthetic. it allows delivery to the ganglion. I ran an informal study prior to bringing this to my patients… we were realistically 90%. Decreased frequency and duration of cluster headaches, migraines… and a case of trigeminal neuralgia. Dolor Technologies distributes the catheter.
December 20, 2018
DebKimberly –
Where are you located?
Do you know of any doctors in Orlando doing this procedure?
Tks.
July 7, 2019
DeanaHi Kimberly, How long do the results typically last for the majority of your patients? My daughter suffered a concussion/whiplash 9 months ago and has had a constant migraine 24/7. She tried the SPG block and had relief but if only lasted 4 hrs and the headache came back much worse. She would try it again but is afraid of a similar result. Just wondering your experience/opinion with this procedure.
Deana
December 20, 2018
DebDenise – Would you mind sharing where you go to get this procedure?
February 16, 2019
Colleen ClarkIs there anyone in Michigan that does SPG?
January 21, 2020
ReinaSPG works great it has been the only thing that has helped with my cluster headaches
February 3, 2020
Debra MullensColleen I to Am from Michigan, Can I ask If you found one and If all WHO.
Thank you
Debbie
April 17, 2019
SandyA friend of mine has been having this procedure done at U of M in Ann Arbor, and McClaren Bay Neurology in Bay City is doing this procudure, as well.
August 27, 2019
Naomi, PA-CIn my office-based practice, I have offered SPG blocks via syringe and angiocath (needle removed) for the past year. I use 0.4 cc of 2% Lidocaine per nostril. A piece of hard candy prior to the instillation of the Lidocaine blunts the bad taste, and the swallowing decreases any numbness.
Some patients have immediate relief, some take 20 minutes, some take close to an hour; but they all (so far) have gotten 3-8 VAS points of relief.
Most patients go on to have reduced number and severity of migraines. The usual schedule of treatment is one block per week for three weeks. After that, the patient returns when their symptoms first begin to resurface –usually 6- 8 weeks later. Repeating the block then typically results in 2-4 months of reduced migraines.
I also administer the block for anxiety and TMJ pain with good results.
I do not pre-numb the nostril nor use a heart monitor. Approximately 10% of patients (usually of Celtic heritage) will feel light-headed upon completion of the block. An additional 3 minutes or so of sitting is usually sufficient to restore them.
SPG blocks are easy and efficacious. Try them !
September 12, 2019
LucyIs the schedule 1 time per week for 3-4 weeks in row normally that general practice for administrating the spg block via SpinoCath?
January 18, 2020
Naomi, PA-CIt is a reasonable schedule. I prefer to perform 3 blocks within 10-14 days. Results seem to last longer with clustered treatments than with them spaced a month or so apart.
February 17, 2020
Dr Ira L ShapiraI have been utilizing Sphenopalatine Ganglion Blocks (SPG Blocks) since 1986. I( teach patients to self-administer the blocks with cotton-tipped catheters that give continual capillary release of lidocaine. Self-Administration give the patient control of their pain relief and allows more frequent use.
The blocks can be used prophylactically to prevent migraines or at the first sign of onset. They decrease suffering and reduce needs for visits to ER for relief.
2% lidocaine is used which has natural anti-inflamatory properties.