The Medicare Access and CHIP Reauthorization Act (MACRA), passed in 2015, was a transformational law. It eliminated the flawed sustainable growth rate formula (SGR) that was used to set Medicare physician payments and created a new quality performance program in Medicare called the Quality Reporting Program (QPP). The QPP includes two participation tracks, the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (AAPMS). Most emergency physicians are in the first track, MIPS, as they do not meaningfully participate in an AAPM, like an accountable care organization (ACO) initiative. MIPS includes four performance categories: quality, cost, improvement activities, and promoting interoperability (formerly meaningful use). Performance on these four categories (which are weighted) roll up into an overall score that translates to an upward, downward, or neutral payment adjustment that providers receive two years after the performance period. MIPS was designed to be budget neutral, and as result of this, the program requires imposing financial penalties on low-performing clinicians’ Medicare reimbursement to pay for incentives for high-performing clinicians.
Explore This Issue
ACEP Now: Vol 41 – No 05 – May 2022What’s Happening with MIPS in 2023?
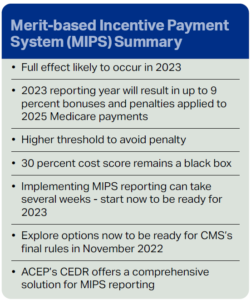
Because of the COVID-19 pandemic, CMS delayed the penalty phase-in and substantive bonus payments, resulting in neutral payment adjustments for the 2020 and 2021 performance years. CMS also approved the Extreme and Uncontrollable Circumstances exclusion for clinicians impacted by COVID-19 for 2022. But, in 2023, the MIPS program likely will resume with full implementation, with up to 9 percent penalties and bonuses for up to half of eligible clinicians.
By design, the 2023 performance year will determine clinicians’ 2025 Medicare Part B payments. In 2025 (payment year), the MIPS program is scheduled to penalize half of the eligible clinicians and reward the other half with bonuses, based on a MIPS score (zero to 100) calculated from the annual submission of 2023 performance data. Implementing a qualified MIPS reporting process can take several weeks, so now is the time to prepare.
The maximum penalty for the 2023 performance year is 9 percent, which is scaled based on the clinician’s MIPS score. Based on the 2021 Final Rule, clinicians will need to score at least 75 (median score) in 2023 to avoid a penalty, with scores above this mark resulting in bonuses. Simply put, CMS expects about half of all clinicians to fall below 75 and receive a penalty.
Will My Group and I Receive a Penalty or a Bonus?
Eligible emergency physicians face several challenges because of an unbalanced playing field in the MIPS program compared to other specialties. First, the most common method for MIPS participation is through a Qualified Registry using CMS-approved, public domain quality measures. However, the public quality measures are more applicable to primary care and require near-perfect performance to obtain even a nominal score. Further, starting in 2022, 30 percent of the MIPS score will be calculated internally by CMS from a “cost score” based on submitted claims. To date, CMS has not provided any insight into how this “cost score” is calculated, so how you and your group will score is impossible to predict. Groups can estimate their total scores by incorporating “cost scores” from a prior year’s performance and combine that with the estimated quality measure scores from the QR or QCDR; however, given the unknown methodology, this approach may not be accurate. Thus, it will not only be harder to score well, but also more challenging to anticipate how your Medicare payments will be impacted.
Should We Report as a Group or as Individuals?
Under MIPS, clinicians may submit as individuals or groups under the same Tax Identification Number (TIN). When reporting as an individual, the MIPS score received only applies to the individual reporting clinician. When reporting as a group, all clinicians who use that TIN receive the same score and payment adjustment based on the entire group’s performance.
Historically, group submissions score higher than individual submissions, so most groups opt for this method to improve their score. Having advance insight into individual and group MIPS scores (whether they are above or below 75) can be used strategically to minimize penalties or maximize bonuses.
However, given the lack of insight into the 30 percent accounted for by the cost score, it becomes higher risk to report as a group in 2023. For example, suppose a group estimates their MIPS score is above 75 and submits as a group, but ultimately (because of the cost score or other factors) receives a MIPS score below 75. In that case, every clinician in the group receives a penalty in the 2025 payment year.
Conversely, suppose a group estimates their MIPS score to be below 75. They may choose to submit as individuals so only the eligible clinicians take the penalty and non-eligible clinicians receive a neutral adjustment. However, if they later discover they would have scored above 75 had they filed as a group, the group effectively “opted out” of bonuses for non-eligible clinicians (under the TIN) and likely secured lower scores at the individual level for the eligible clinicians.
Are There Other Options to Participate in QPP Outside of MIPS?
Participation in the QPP is mandatory for all clinicians receiving Medicare reimbursement.
- Clinician groups can participate in QPP as part of an advanced alternative payment model track—for example, by reporting as a member of an ACO, since AAPMs are not subject to the same financial penalties as MIPS. Historically, many emergency physicians have been excluded from APMs or ACOs. In addition, reporting as an advanced APM requires advanced planning, time, and resources.
- Groups might also participate using their hospital’s Value-Based Purchasing (VBP) program scores. Historically, some EM groups do well through this program, but how the VBP score translates into a MIPS score is not revealed by CMS until after MIPS submissions.
QR/QCDR Participation Is Costly. What Can I Do to Minimize Losses?
Emergency physician groups have several complex considerations in the 2023 performance year to minimize financial loss or maximize financial bonuses in 2025. For example, groups with fewer eligible clinicians may have less exposure to both penalties or bonuses, which may not outweigh the substantial resources needed for quality measurement and reporting.
If a group’s objective is to simply minimize financial losses (including time and resources invested into QR/ QCDR reporting), they might choose to merely submit “improvement activities” directly to CMS for eligible clinicians and not report any quality measures as individuals. Eligible clinicians would likely receive a penalty for 2025, but it would probably be less than the 9 percent maximum penalty.
In addition, some EM billing companies offer quality registry reporting as part of their service. QRs may be less resource intensive; however, QR reporting is limited to public domain quality measures which are less applicable to EM. Therefore, reporting through QRs may not offer confidence for a bonus-eligible score given competition with clinicians from other specialties on non-emergency medicine measures. However, reporting of measures through the QR may reduce the penalty exposure of a group.
How Can We Maximize Payments and Bonuses?
If a group’s objective is to maximize financial gain, the MIPS score and resulting bonus payment must exceed the cost of the reporting mechanism used. Groups can submit data via third party intermediaries such as a Quality Registry (QR) or a Qualified Clinical Data Registry (QCDR). While QRs may be less resource-intensive, groups would need to achieve near-perfect performance relative to all clinicians participating in MIPS (across specialties) to avoid a penalty or receive a bonus. Alternately, groups may invest in reporting through a QCDR, which offers EM-specific measures as an alternative to the generic public domain measures. ACEP’s Clinical Emergency Data Registry (CEDR) is one commonly used QCDRs offering custom emergency medicine focused QCDR quality measures. Historically, EM groups participating in MIPS outside of QCDRs have some of the lowest scores among MIPS-eligible clinicians.
Targeting an estimated MIPS score well above 75 would provide confidence in avoiding penalties, as well as offsetting the cost of reporting by the bonus payments received for both eligible and not eligible clinicians.
Pages: 1 2 | Single Page





No Responses to “MIPS 2023: Prepare Now to Avoid Financial Penalties”