
Explore This Issue
ACEP Now: Vol 35 – No 03 – March 2016(click for larger image) Table 1. Average Cost of Naloxone by Type and Dose
Means of Distribution
Providers can provide naloxone directly to patients, write a prescription, or refer patients to a community organization or pharmacy participating in a collaborative practice agreement. Prescribing is low-impact to the system and can be implemented immediately.
Naloxone is offered in intramuscular (IM) and intranasal (IN) formulations. IM can be delivered in the lateral arm or thigh. IN is given as a spray in each nostril with similar efficacy and safety.12,13
IM naloxone can be dispensed as two single-dose vials, 0.4 mg/mL, with syringe and needles. Approved by the US Food and Drug Administration (FDA), Evzio is a prefilled auto-injector that contains a single dose of naloxone 0.4 mg.14 IN naloxone is prescribed as a 2 mL prefilled luer-lock needleless syringe with an IN mucosal atomizing device.15 The recently FDA-approved Narcan is a preloaded nasal atomization device that delivers a single 4 mg dose. This higher dose is necessary for IN route of delivery and for patients who do not respond to the lower dose (e.g., after fentanyl overdose). With the exception of the preloaded IN device, it is recommended that you prescribe two naloxone doses.
Cost
ED naloxone programs may be funded through your hospital, grants, or local governmental agencies. Public health departments and community-based naloxone programs can also be key allies. Depending on your state, Medicaid may reimburse for the naloxone kit and/or overdose education.
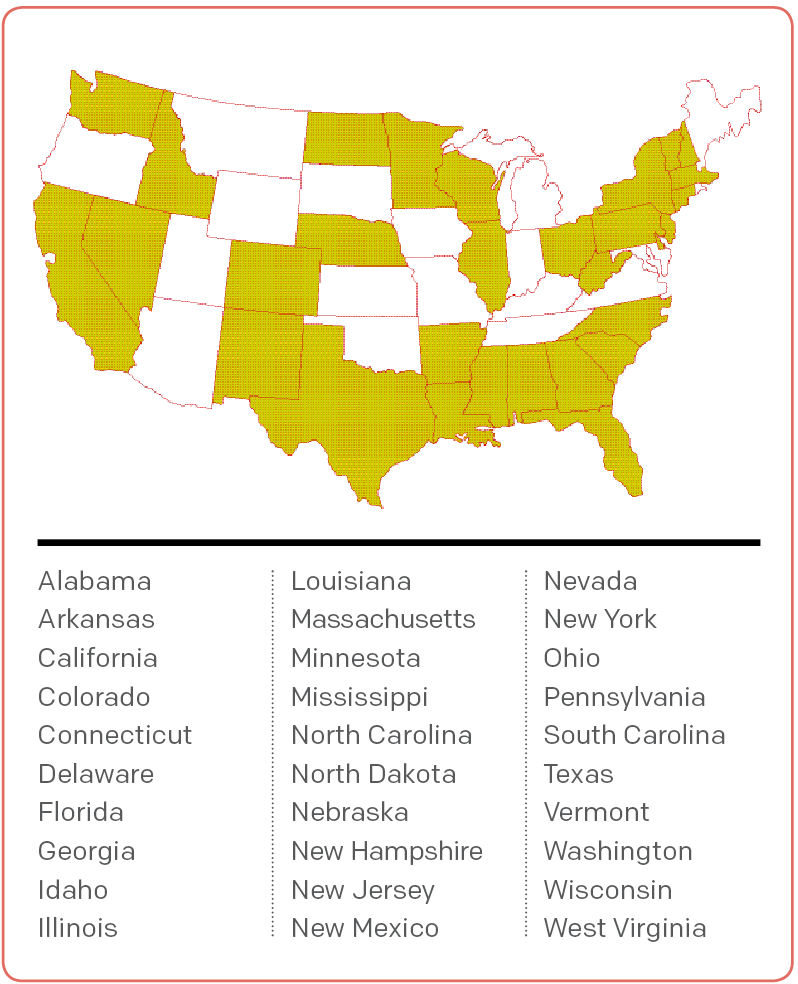
Figure 1. States With Legislation Preventing Prescribers From Being Criminally Liable for Prescribing, Dispensing, or Distributing Naloxone to Laypeople
Source: Law Atlas.
The cost of naloxone ranges by manufacturer (see Table 1). The Evzio auto-injector may also be covered by insurance or Kaléo’s patient assistance program.16 To accurately estimate cost, first estimate need and then select items for your naloxone kits. Take-home naloxone kits are given to patients or their loved ones for out-of-hospital use in case of an overdose and may include educational materials, nasal atomizers or needle and syringes, gloves, face shield, and two doses of naloxone.
Patient Education
Patient education should cover overdose risk factors, avoiding overdose, recognizing and responding to an overdose, and administration of naloxone. A combination of in-person counseling and an educational video or handout is best, if feasible. Family and friends should be included in the training, as they may be administering naloxone in an out-of-hospital overdose.
Pages: 1 2 3 4 | Single Page





One Response to “Naloxone Distribution Strategies Needed in Emergency Departments”
April 3, 2016
Larry A. Bedard, MD FACEPACEP has come a long way since 2010 when a wacko doctor from California-me- introduced resolutions to have naloxone over the counter and recommend EPs prescribe naloxone in the ER.
However, ACEP still has a long way to go. Tp deny our role in the opiod epidemic, while frequently blaming other specialities for the epidemic is the wrong approach.