
Explore This Issue
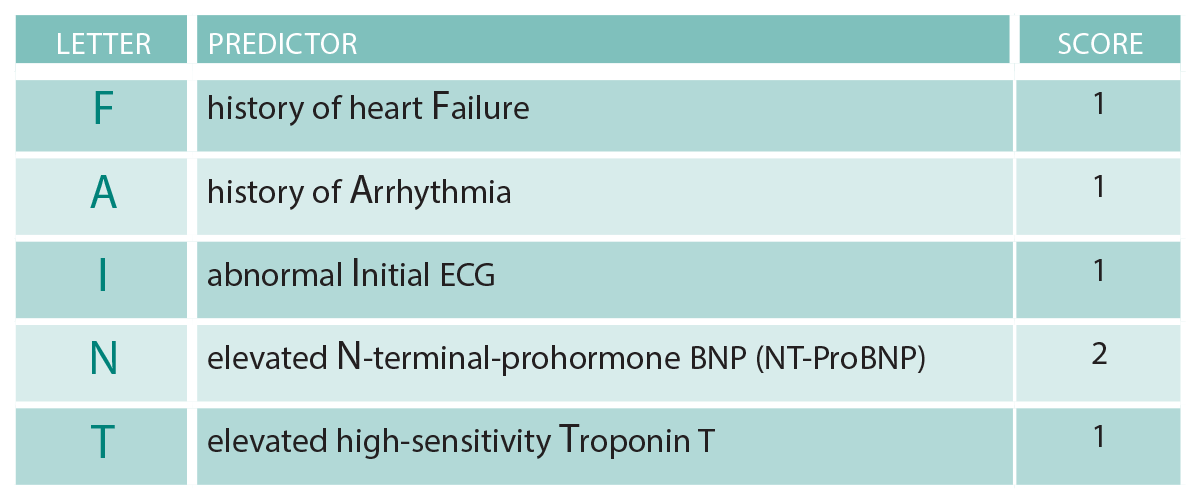
ACEP Now: Vol 38 – No 12 – December 2019(click for larger image) Table 1: FAINT Score1
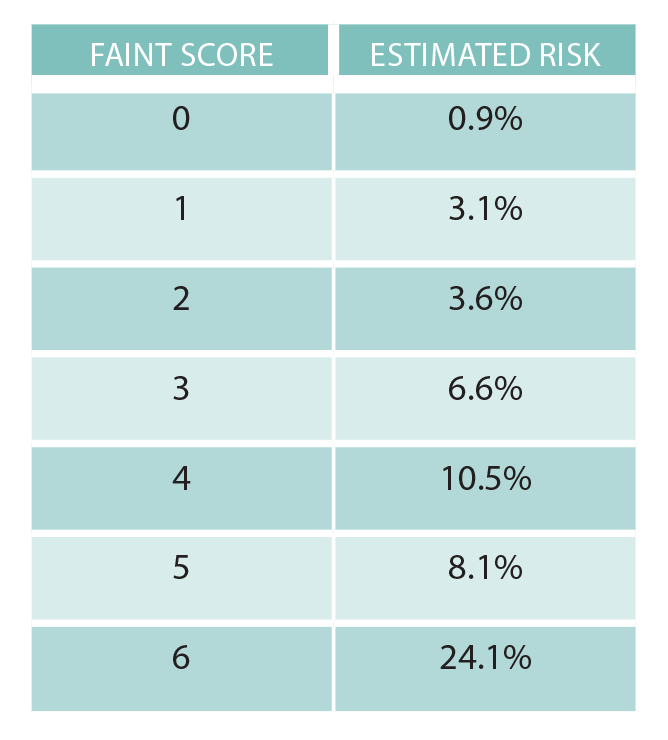
The negative predictive value of a FAINT Score of zero was over 99 percent, a promising finding that should satisfy those clinicians who believe that 1 percent is generally an acceptable miss rate for patients presenting with cardiovascular complaints. However, this risk score has not been externally validated and thus is not ready for clinical use in isolation.
The FAINT Score now joins its Canadian cousin from Ottawa, the Canadian Syncope Risk Score. The latter has a greater number of variables (nine), some of which are subjective (ED diagnosis of cardiac syncope, for example), and is designed for use in patients ages 16 and older. Not surprisingly, both scores use the ECG and troponin as important predictive variables.
What’s next? Both scores are pending external validation to confirm that their test characteristics are, in fact, consistent with those in the initial derivation studies. Meanwhile, the formal external validation of the Canadian score is expected to be published soon.
The validation of the FAINT Score is likely a few years away. Until then, we cannot formally endorse the use of it for widespread implementation. However, these scores are an exciting new development in the field of syncope risk stratification and may offer clinicians a useful tool to help determine which patients can be safely discharged directly from the emergency department. Ultimately, we believe these scores should be used in conjunction with, and not instead of, clinical gestalt, as is true for all clinical decision instruments. Consideration of other factors—such as the social circumstances, patient values, and preferences—is always warranted.
Case Resolution
Since the FAINT Score has not yet been externally validated, you cannot rely solely upon it. But its components may still be useful. You aptly order a high-sensitivity troponin and elevated N-terminal-prohormone BNP (NT-ProBNP), both of which come back normal. Calculating the patient’s FAINT Score to be zero, you believe that her risk of a serious cardiac event within 30 days is likely to be less than 1 percent. You return to the bedside and engage in shared decision-making with the patient. She understands that her risk is probably low but not zero. Although she lives alone, she agrees that discharge home with close outpatient follow-up this week is appropriate. The etiology of the syncope is never determined, but months later she is doing well, safely drinking coffee in her living room.
Pages: 1 2 3 | Single Page





One Response to “New “FAINT” Score May Work for Syncope Risk Stratification, but Needs Validation”
December 28, 2019
KazmiExcellent. Thanks. -Needs more to add to,it. D/D seizure. Then this. Check orthostatic BP. The best thing is that all ER personnel should start using this and keep on adding things which are necessary to improve this. I am going to start using this and try to improve and add my own pointers.