
Recent data published in Pediatrics reveals racial/ethnic and socioeconomic disparities of COVID-19 among children.6 Among 1,000 children tested at a drive-through/walk-up testing site within one mile of Children’s National Hospital in Washington D.C., the demographic breakdown of children who tested positive was 46 percent Latinx, 30 percent Black, and 7 percent white. Of the children who tested positive, 9 percent were children from families in the highest income quartile and 38 percent were in the lowest income quartile. These results corroborate findings published in JAMA from the Johns Hopkins Health System, which found that of 37,727 patients tested for COVID-19, the positivity rate was 42.6 percent for Latinx patients and 17.6 percent for Black patients.7 To date, no data suggest that presenting symptoms of COVID-19 among children differ by race/ethnicity or socioeconomic status.
Explore This Issue
ACEP Now: Vol 39 – No 09 – September 2020Children tend to have less severe disease compared to adults. The CDC estimates the rate of hospitalization among children at 8.0 per 100,000 compared to adults at 164.5 per 100,000 population, with similar lower rates of mechanical ventilation and death.2 Children with symptomatic COVID-19 often have nonspecific symptoms, including vague respiratory or only gastrointestinal symptoms. The most common presenting symptoms are cough and/or fever.2 However, almost one-third of children admitted to the hospital are admitted to intensive care units.8
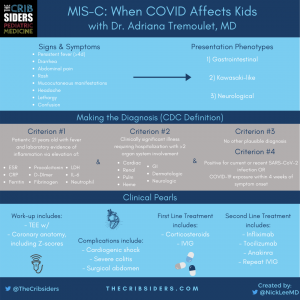
Multisystem Inflammatory Syndrome
A new complication of COVID-19 that is particularly devastating is the multisystem inflammatory syndrome in children (MIS-C).9 While rare, it has received attention. The American College of Rheumatology defines MIS-C as an postinfectious inflammatory syndrome characterized by fever, inflammation, and multiorgan dysfunction that occurs late in the course of COVID-19 in children.10 The new FOAMed website and podcast The Cribsiders (https://thecurbsiders.com/thecribsiders), led by internists and pediatricians from 15 different institutions across the country, recently published an episode dedicated to MIS-C.11 In brief, the presentation of MIS-C seems to have three common phenotypes: Kawasaki-like, gastrointestinal, and neurologic. In Figure 1, the signs and symptoms, evaluation, and management of MIS-C are summarized. Interestingly, data from the CDC reveals that MIS-C is more prevalent among Latinx (38 percent) and Black (33 percent) children compared to white (15 percent) children.12
Finally, with respect to COVID-19 treatment, the evidence for children in the United States (and elsewhere) is an evolving area of research. Treatments for moderate-to-severe COVID-19, such as remdesivir and dexamethasone, have not been fully evaluated in children of different age groups. What is clear, however, is that children are vectors of the SARS-CoV-2 virus. They may be asymptomatic or have non-specific symptoms, and a smaller subset can become quite ill from the acute illness or later as a result of MIS-C.
References
- Coronavirus disease 2019 in children—United States, February 12–April 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(14):422-426.
- Care for children. Centers for Disease Control and Prevention website. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/pediatric-hcp.html. Accessed Sept. 1, 2020.
- Bunyavanich S, Do A, Vicencio A. Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA. 2020;323(23):2427-2429.
- Heald-Sargent T, Muller WJ, Zheng X, et al. Age-related differences in nasopharyngeal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) levels in patients with mild to moderate coronavirus disease 2019 (COVID-19) [published online ahead of print, July 30, 2020]. JAMA Pediatr. doi:10.1001/jamapediatrics.2020.3651.
- Sola AM, David AP, Rosbe KW, et al. Prevalence of SARS-CoV-2 infection in children without symptoms of coronavirus disease 2019 [published online ahead of print, Aug. 25, 2020]. JAMA Pediatr. doi:10.1001/jamapediatrics.2020.4095.
- Goyal MK, Simpson JN, Boyle MD, et al. Racial/ethnic and socioeconomic disparities of SARS-CoV-2 infection among children [published online ahead of print, Aug. 20, 2020]. Pediatrics doi: 10.1542/peds.2020-009951.
- Martinez DA, Hinson JS, Klein EY, et al. SARS-CoV-2 positivity rate for Latinos in the Baltimore–Washington, DC region. JAMA. 2020;324(4):392-395.
- Kim L, Whitaker M, O’Halloran A, et al. Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory-confirmed COVID-19 — COVID-NET, 14 States, March 1–July 25, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1081-1088.
- Multisystem inflammatory syndrome (MIS-C). Centers for Disease Control and Prevention website. Available at: https://www.cdc.gov/mis-c. Accessed Sept. 1, 2020.
- Henderson LA, Canna SW, Friedman KG, et al. American College of Rheumatology clinical guidance for pediatric patients with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 and hyperinflammation in COVID-19. Version 1 [published online ahead of print, July 23, 2020]. Arthritis Rheumatol. doi:10.1002/art.41454.
- Berk J. #5 MIS-C: when COVID affects kids. The Curbsiders website. Available at: https://thecurbsiders.com/cribsiders/5. Accessed Sept. 1, 2020.
- Multisystem inflammatory syndrome (MIS-C): cases in the U.S. Centers for Disease Control and Prevention website. Available at: https://www.cdc.gov/mis-c/cases/index.html. Accessed Sept. 1, 2020.
Pages: 1 2 3 | Single Page





No Responses to “New Research Broadens Our Understanding of COVID-19 in Kids”