
A literature review identified multiple interacting variables that affect the MUR.9 The following variables (see Table 1) contribute significantly to the PPRs: ambient temperature, event type, event duration, crowd mood, crowd density, attendance, average age, and the prevalence of alcohol and drug use. Cold and rainy days generally lead to lower PPRs but with a higher incidence of hypothermia, frostbite, and falls, while hot weather leads to higher PPRs for dehydration, insect bites, and sunburns.9 Rock concerts have a positive correlation with trauma (often secondary to moshing and crowd surfing).9 At music concerts, attendees often have limited mobility and consume drugs and excessive amounts of alcohol, leading to higher PPRs. Event duration extends exposure and increases exhaustion.9 Crowd density may affect crowd mood, limit access of patrons to water and facilities, and limit EMS access to potential patients.9 Interestingly, PPRs tend to decrease with higher attendance (ie, as the number of spectators increases, the number of patients evaluated per 10,000 in attendance decreases).9 The reasons for this are not understood.
Explore This Issue
ACEP Now: Vol 36 – No 04 – April 2017Younger adult spectators use more alcohol and drugs than older spectators and have increased trauma, often secondary to physical altercations.9 Age distribution of a particular event is also a key variable as medical and social issues for older patrons differ widely from those of younger crowds due to their behavior, judgment, frailty, and vulnerability.9
Heat index is associated directly with PPRs.13 The heat index at the kickoff times of football games in the southeastern United States was compared to the PPRs for the games over the course of four years. For every 10-degree increase in the heat index, three more patients per 10,000 patrons required medical care.
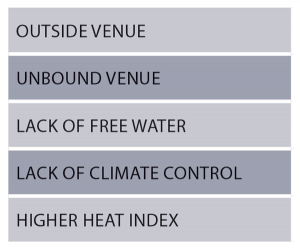
Table 2: Variables That Predict Increased Patient Presentation Rate
Five variables (see Table 2) are known to increase PPR: unbounded venues, outdoor venues, events lacking free water, lack of climate control, and a higher heat index. 5 Thus, medical staffing should be especially prepared if these risk factors exist. After accounting for these other variables, the presence of alcohol does not increase the PPR.
Conclusion
The following actions can improve patient safety at mass gatherings as described in a recent prospective analysis of patients at a large outdoor summertime mass gathering: develop and drill incident action plans in preparation for disaster scenarios and mass casualty incidents; use roaming, clearly identified medical staff; provide free water for attendees; designate multiple access points for EMS in the event of transport or a mass casualty incident; and use trained medical staff capable of administering rapid cooling, benzodiazepines, and advanced airway management, including rapid sequence intubation.14
Pages: 1 2 3 | Single Page





No Responses to “Onsite Medical Care, Resuscitation Increasingly Important at Mass Gathering Events”