Explore This Issue
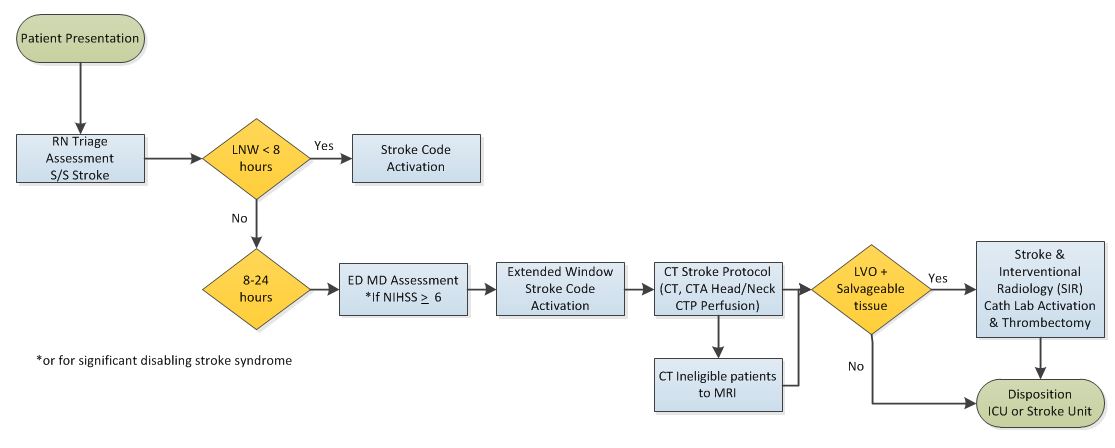
ACEP Now: Vol 37 – No 04 – April 2018Stanford University’s Stroke Code Extended protocol.(Click for larger image.)
Source: Alexei Wagner
Other unique protocol elements include expedited CT angiogram and perfusion imaging, and mobilization of the interventional neuroradiology team for thrombectomy. The CT angiogram and perfusion imaging is critical in determining the amount of brain tissue at risk of infarct, and therefore whether thrombectomy would be indicated. To determine patients appropriate for thrombectomy with adequate salvageable tissue, the team looks at the ratio of ischemic tissue to the initial infarct volume (ischemic core), and an absolute volume of potentially reversible ischemia (penumbra).
The Stroke Code Extended also requires the emergency department attending to perform and document a NIHSS score on all suspected stroke patients. Although this is a core emergency medicine skill, Stanford instituted an educational initiative to certify our entire faculty and residency in performing the assessment. This was accomplished through online training modules and traditional lecture-style didactics.
In addition, immediately upon arrival at the bedside, the neurology resident now performs an NIHSS stroke scale assessment. Our goal is to study the inter-rater reliability between neurology- and emergency medicine-completed NIHSS stroke scales.
Beyond the New Protocol
Parallel to our initiative to identify and treat extended strokes, Stanford’s neurology department has performed significant educational outreach to referral hospitals to facilitate the rapid transport of stroke patients to Stanford Hospital even if they’re outside the tPA window but still likely to benefit from thrombectomy. In addition, the Stanford School of Medicine has found that collaboration between the emergency medicine and neurology departments is instrumental in improving the treatment of acute stroke.
Looking ahead, we will evaluate the implementation of this protocol by collecting stroke quality metrics, measuring NIHSS inter-rater reliability, and monitoring the stroke mimic rate. We look forward to sharing further insights about our protocol and results.
 Dr. Wagner is assistant director of Adult Emergency Medicine at the Stanford University School of Medicine in Palo Alto, Calif.
Dr. Wagner is assistant director of Adult Emergency Medicine at the Stanford University School of Medicine in Palo Alto, Calif.
 Dr. Shen is the interim chair of the Department of Emergency Medicine at the Stanford University School of Medicine in Palo Alto, Calif.
Dr. Shen is the interim chair of the Department of Emergency Medicine at the Stanford University School of Medicine in Palo Alto, Calif.
References
- Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11-21.
- Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708-718.
Pages: 1 2 3 | Single Page





No Responses to “Opinion: Stanford’s New Stroke Protocol Expands the Treatment Window”