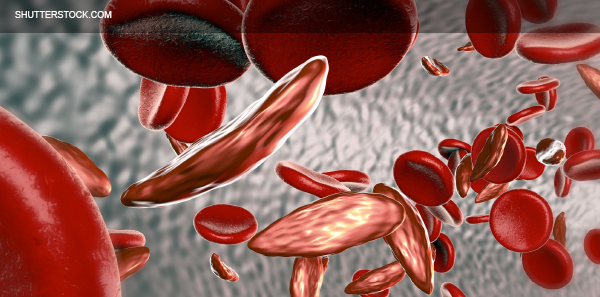
Sickle cell disease (SCD) is an inherited hemoglobin disorder that affects approximately 100,000 individuals in the United States. Disease hallmarks include chronic hemolytic anemia, progressive organ damage, and, most notably to the emergency physician, pain. SCD causes pain in several ways. Acute episodes, caused by vaso-occlusion, last days to weeks at a time, whereas chronic pain commonly involves bony causes such as avascular necrosis and bone infarcts. Because disease-modifying therapies can reduce but not eliminate SCD pain, opioids have been a cornerstone of SCD pain management for decades. Amid today’s opioid epidemic where physicians are forced to be more cautious in their dispensation and administration of opioids, people with SCD experience new challenges in accessing opioids from emergency providers during acute pain episodes. We now know that opioids are more dangerous than previously recognized. This raises the question, should emergency physicians stop or reduce their use of opioids for SCD pain in the emergency department?
Explore This Issue
ACEP Now: Vol 36 – No 12 – December 2017My clinical practice offers a unique perspective on this matter. While my formal training (and board certification) is in emergency medicine only, I designed, for myself, additional SCD-specific clinical training after residency and have pursued a research career focused on SCD. In 2012, I took over the adult SCD clinic at Mount Sinai in New York, which gave me the opportunity to practice both general emergency medicine and outpatient SCD care. In 2012, the clinic cared for 40 patients. Our census has now grown to more than 200 adults, and we have overseen substantial reductions in per-capita ED utilization, admission rates, and hospital length of stay. I attribute much of our success in reducing acute-care utilization to our relentless outpatient efforts to minimize long-term opioid use and rapidly identify aberrant behaviors and opioid misuse before they get out of control. Complying with new government regulations regarding opioid monitoring and prescribing has not been a problem for my practice because our protocols generally exceed these requirements. That being said, my clinic still prescribes a tremendous number of opioids (both long- and short-acting) because, until our disease-modifying SCD therapies improve, opioids are still indicated as first-line therapy for SCD pain. To the question of whether emergency physicians should reduce or restrict their use of opioids for acute sickle cell pain, my answer is that while dispensation of prescriptions should be limited, use of IV opioids in the emergency department should continue or (at some institutions) even increase.
Until our disease-modifying SCD therapies improve, opioids are still indicated as first-line therapy for SCD pain.
Reasons physicians may withhold opioids during an ED visit are many, and physicians have had reservations about giving opioids to people with SCD long before the prescription opioid crisis. Based on a 2011 study of emergency provider attitudes by my colleagues and me, fears of facilitating addiction or aberrant drug behaviors, concerns that patients with SCD overreport or exaggerate pain, and the belief that people with SCD are manipulative were issues that topped the list.1 For the majority of SCD patients (where the average number of ED visits per year ranges from one to three), opioid misuse is not an issue, and acute attacks of SCD pain should be treated aggressively with IV opioids. The new context of the opioid epidemic may encourage ED providers to withhold opioids more often during ED visits for SCD, but it shouldn’t. A minority of high-utilizing patients with SCD account for the majority of SCD visits, and for these people, concerns about addiction and inappropriate narcotic cues may be well-founded. However, withholding opioids in the emergency department before a comprehensive evaluation has been performed is not appropriate. Josh Field’s publication in the American Journal of Hematology describes how intensive management (which involves a careful assessment of an individual’s reasons for overutilization of the emergency department before opioids are withheld) can safely reduce excess ED visits.2
Pages: 1 2 | Single Page




No Responses to “Are Opioids for Sickle Cell Disease Appropriate, or Do They Enable Addiction?”