Equipment list and tips on technique for the ED physician
Case
A 58-year-old male patient presents to the triage area of your ED with the complaint of coffee ground emesis. He has end-stage liver disease from HCV cirrhosis and is on the liver-transplant list. His blood pressure is 105/70, his heart rate is 105, and his abdomen is large and distended. Despite the patient’s slightly abnormal vitals, you feel in your gut that this patient is really sick and will decompensate quickly if not aggressively managed. Your first priority is to protect his airway, so you quickly review your intubation checklist (emcrit.org/airway) and set up for the tube.
Explore This Issue
ACEP Now: Vol 33 – No 01 – January 2014Knowing the patient has a belly full of blood, you place an NG-tube and suck out a liter of clotted blood. Using a small dose of ketamine and a large dose of rocuronium, you perform RSI using video laryngoscopy. Thankfully, there is no aspiration, and the patient’s vitals remain stable in the peri-intubation period.
Ten minutes later, however, the patient’s blood pressure worsens. He is still bleeding, and his labs show a low hemoglobin level, coagulopathy, and thrombocytopenia. You initiate your hospital’s massive transfusion protocol and replace the patient’s 18-gauge with a rapid-infusion catheter, a large bore catheter that is placed over a wire inserted through an existing peripheral IV.
You start a ketamine drip, along with octreotide, antibiotics, and tranexamic acid (based solely on evidence extrapolated from the trauma literature). You call GI for endoscopy, but they won’t be in for another 45 minutes. Despite receiving 10 units PRBC, 8 units FFP and two packs of platelets through a level-one infuser, the patient continues to bleed, and his blood pressure continues to drop. You know your next step is placing a Blakemore tube, but how do you put one in?
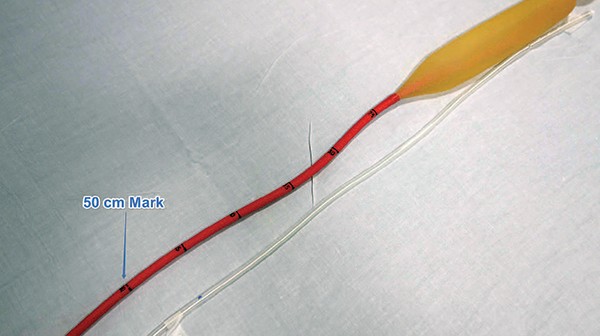
Although most of us know that Blakemore placement is the next step to temporize massive UGIB from esophageal varices, few have ever placed one and their use is not intuitive. It is crucial to rehearse the steps of placing a Blakemore in your mind and ensure you have all the requisite supplies available in your ED before a sick GI bleeder rolls in.
Pages: 1 2 3 | Single Page





No Responses to “How To Place A Blakemore Tube in an ED Patient with Upper GI Bleeding from Esophageal Varices”