Explore This Issue
ACEP Now: Vol 33 – No 05 – May 2014An interview with reimbursement and coding expert Michael Granovsky, MD, CPC, FACEP

When it comes to compensation, good documentation is a physician’s best friend.
Increasingly, emergency physicians find that anywhere from 30 to 50 percent of their compensation is based on RVU production. Some groups have even adopted 100 percent RVU-based compensation models, said Michael Granovsky, MD, CPC, FACEP, president of Logix Health, a national ED billing company. Without adequate and thorough documentation of evaluation and management (E/M) services, providers risk losing RVUs and having payments reduced for the care they provide.
It pays for physicians to take notice.
As much as 89 percent of the revenue in the ED comes from the E/M codes level 1 (92281) to level 5 (92285) and critical care.
An emergency physician would expect to be compensated less for seeing a patient with a simple bee sting than for seeing a patient with severe chest pain. However, the physician who does not adequately document the chest pain case may find it downcoded. A level 5 downcoded to a level 3 represents a loss of 64 percent of the RVUs and is roughly equivalent to providing a level 4 service for free.
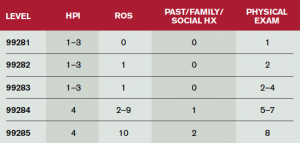
The insurance companies will not see the patient’s chart, thus it is up to physicians to empower coders with adequate documentation to report the appropriate code for services provided. The number-one way to ensure this is to provide the documentation required by the Medicare 1995 documentation guidelines appropriate for the care delivered (see Table 1).
It’s important to note that doesn’t mean overdocumenting.
“You can’t take an ankle sprain and document it excessively, and it magically becomes a level 5,” said Dr. Granovsky. “We are seeing a significant increase in audit activity targeting the overuse of macros.”
Three primary elements factor into determining the E/M level of a case: history, physical exam, and medical decision making.
History is composed of chief complaint; history of present illness (HPI); review of systems (ROS); and past medical, family, and/or social history.
The minimum number of HPI elements for E/M levels 4 and 5 is four, and failure to meet this is the single most costly documentation error. Dr. Granovsky recommended that the rich clinical detail in the HPI become one of the tools physicians use to paint a clear clinical picture in what otherwise might be a bland electronic medical record (EMR) history and physical exam.
Pages: 1 2 | Single Page





No Responses to “Prevent Loss of RVUs, Reduced Physician Compensation by Properly Documenting Evaluation and Management Services in the Emergency Department”