
Explore This Issue
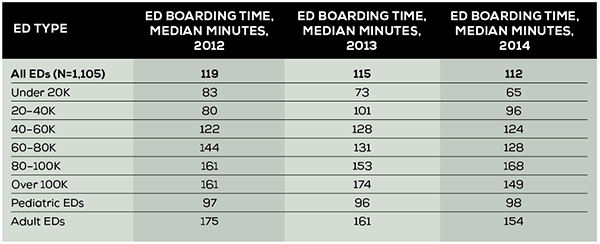
ACEP Now: Vol 34 – No 12 – December 2015(click for larger image) Table 1. Boarding Time in the EDBA Data Survey Through 2014
But in many EDs, and in particular those in the 20,000 to 60,000 cohorts, the boarding time has actually increased over the three years measured. There is clearly an opportunity gifted from CMS and The Joint Commission to allow ED leaders the traction needed to negotiate better hospital flow for admitted patients. More ED physicians and nurses need to engage in the efficient processing of patients needing inpatient services. In most hospitals, this will primarily be focused on patients being admitted to the same hospital, which on average is 17 percent of overall ED volume. But processes will also facilitate the movement of patients to admission units of other hospitals when transfers are necessary, which is about 2 percent of patients in the average ED.
Boarding of inpatients in the ED leads to crowded conditions, lack of patient care areas, insufficient staff to process all ED arrivals, and then a deadly cascade. The cascade will typically include prolonged patient waiting times, increased suffering for those waiting for service, unpleasant treatment environments, ambulance diversion, and poor patient outcomes. The cascade then leads to dissatisfied ED staff, frustration, and turnover at all levels. Overwhelmed EDs also lack the capacity to respond to community emergencies and disasters.
The timely processing of patients who are admitted to the hospital or transferred for admission to another hospital improves the overall flow rate of all ED patients. This leads to a culture of timeliness and satisfaction for all patients who arrive for ED service and reduces walkaway rates.
Where have EDs had success in improving admission flow? Primary work is done outside of the ED, with the global recognition that reduced boarding times are associated with reduced overall hospital length of stay, improved quality of care, and closer adherence to established hospital pathways. ED nursing leadership needs to focus its efforts on the nursing administration to link rapid flow of inpatients to nursing incentives. These may be financial (credit for nurse worked hours going to the inpatient unit rather than the ED), communication enhancement (timesaving patient turnover methods from ED to inpatient nurses), and/or recognition (award programs for competing nursing units).
On the physician side, most EDs now admit the majority of patients to hospitalists or group practices, including resident teams. The emergency physicians have the opportunity to negotiate with those services regarding the elements of improved patient service and pathway compliance. Many admitting physicians want a patient to be completely “worked up” by the time that patient will reach the floor and have the most important therapies started. The emergency physician can offer those elements if the admitting service will provide a timely response to emergency physician calls, a rapid concordance on the need for admission, and the timely delivery of an “order to admit.” The emergency physician also needs to facilitate the work of the admitting physician with an organized and complete history and physical exam on the patient record and transition-of-care communication that is clear and concise.
Pages: 1 2 3 | Single Page






No Responses to “Reducing Boarding Time in the Emergency Department Can Improve Patient Care”