Case Resolution
The patient is given LMWH and has outpatient injections arranged. He is referred back to his oncologist to further discuss the issue of using a DOAC to manage his cancer-associated DVT.
Explore This Issue
ACEP Now: Vol 38 – No 01 – January 2019Thank you to Dr. Anand Swaminathan, assistant professor of emergency medicine at the St. Joseph’s Regional Medical Center in Paterson, New Jersey.
Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.
References
- Lee AY, Levine MN, Baker RI, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146-153.
- Beam DM, Kahler ZP, Kline JA. Immediate discharge and home treatment of low-risk venous thromboembolism diagnosed in two U.S. emergency departments with rivaroxaban: a one-year preplanned analysis. Acad Emerg Med. 2015;22(7):788-795.
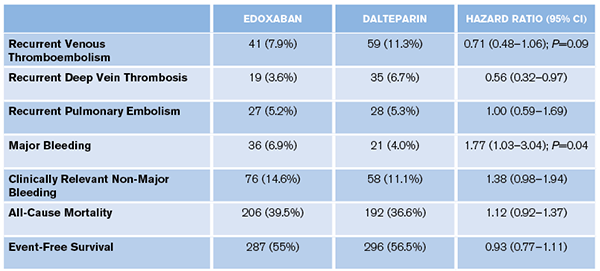
- Young AM, Marshall A, Thirlwall J, et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: results of a randomized trial (SELECT-D). J Clin Oncol. 2018;36(20):2017-2023.
Pages: 1 2 3 | Single Page






One Response to “Should You Use Direct Oral Anticoagulants for Cancer-Associated VTE?”
January 20, 2019
Gregg ChesneyThanks for this review! I had this exact debate last week (but enoxaparin vs rivaroxaban) with our ED pharmacist, the patient’s oncologist and his general surgeon for a patient with an acute DVT 2 weeks post-op from a resection of a colonic adenocarcinoma. I hadn’t seen the new article in the NEJM yet, and the 2016 ACCP VTE guidelines are still recommending LMWH. I had originally ordered enoxaparin but the oncologist decided he wanted to manage him on rivaroxaban, citing new data that DOACs are noninferior in these patients, which I hadn’t had a chance to look for yet, so thanks for filling me in!