We were wrapping up a peaceful shift, as peaceful as it can be for a Level 1 trauma center, when we heard the dreaded overhead page, “Medical alert to red 3.”
Explore This Issue
ACEP Now: Vol 36 – No 11 – November 2017
We entered the room to find a 52-year-old female with the chief complaint of posterior headache for one week, migrating, variable in intensity, but constant and associated with nausea. Well, why was this a medical alert again? The triage nurse added, “Weakness, numbness and tingling to the left upper extremity, onset yesterday morning; dropped tea cup from left hand; slight unsteadiness in left leg, onset yesterday.” The patient added, “I have numbness around my mouth, and I think my vision is off, but that’s been forever! It’s probably nothing. I don’t want to waste your time.”
Background
Cerebral venous sinus thrombosis (CVST) is a type of stroke in which the venous channels of the brain become thrombosed, resulting in cerebral infarction in the areas corresponding to the thrombosis. CVST is uncommon. However, the epidemiology is difficult to determine. One consensus opinion indicates that there is approximately one CVST stroke to every 62.5 arterial thrombotic strokes, while another states that CVST constitutes 0.5 percent to 1 percent of all strokes in young or middle-aged adults.1,2 It is more common in neonates and young persons, with the incidence decreasing as age increases.3 There is a female predominance, with roughly a 3:1 female-to-male ratio, which is influenced by gender-specific factors such as oral contraceptive use, pregnancy, puerperium, and hormonal replacement therapy. Also, women have a better prognosis when CVST is attributable to those factors.3,4
Presentation

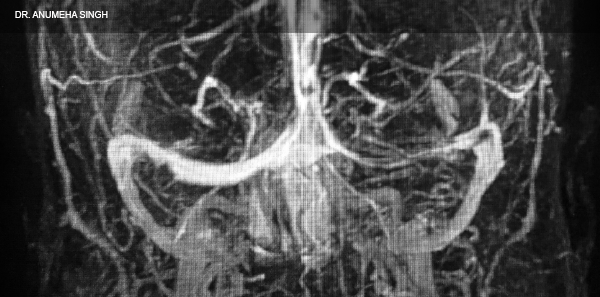
MRI of the 52-year-old female patient with cerebral venous sinus thrombosis.
Source: Dr. Anumeha Singh
Presentation can vary greatly depending on the location and extent of the thrombosis. It can present just with findings suggesting increased intracranial pressure (eg, idiopathic intracranial hypertension), such as headache, vomiting, papilledema, and visual disturbances. Cranial nerve involvement may also be present and include such findings as facial weakness; deafness; visual deficits; or oculomotor, abducens, or trochlear nerve palsies with paralysis of extraocular muscles or ptosis.1 Headache is the most common presenting symptom and is usually localized and gradual in onset. Focal deficits may occur bilaterally, and seizures may occur.3
CVST can also present similarly to encephalopathy with multifocal signs, mental status change, stupor, coma, cognitive dysfunction, frontal lobe syndrome, etc.3
Parenchymal brain lesions depend upon the location and number of occluded sinuses or veins. This can lead to cerebral edema, infarction, or hemorrhagic infarction, which may manifest with motor and sensory deficits, cranial nerve palsy, aphasia, and seizures.3
Diagnosis
American Heart Association/American Stroke Association 2011 guidelines recommend cerebral venous imaging in cases of lobar intracerebral hemorrhage of otherwise unclear origin, cerebral infarction that crosses typical arterial boundaries, and clinical features consistent with idiopathic intracranial hypertension.2 MRI plus magnetic resonance venography is considered the most sensitive modality. CT venography can be considered when MRI is unavailable or contraindicated. If diagnosed, screening for prothrombotic conditions is suggested as well. This typically prompts both neurology and hematological evaluation.3,5,6
Prognosis
Approximately 5 percent of patients die during the acute phase (interval from symptom onset to diagnosis fewer than 48 hours).7,8 Predictors of mortality at 30 days are depressed consciousness, altered mental status, thrombosis of the deep venous system, right hemispheric hemorrhage, and posterior fossa lesions. The primary cause of death is transtentorial herniation. The following are also predictive of poor outcomes: central nervous system infection, malignancy, hemorrhage, Glasgow Coma Scale score less than 9 on admission, age greater than 37 years, and male gender. Complete recovery is expected in 79 percent of the entire cohort.7
Natural Progression
Recanalization occurs in 40 percent to 90 percent of cases, most within four months. The highest rates are in deep cerebral veins and cavernous sinuses. The lowest rates are seen in the transverse or lateral sinuses. Recurrence rates for CVST are 2 percent to 4 percent, with increased risk in males, prothrombotic states, thrombophilia, polycythemia, and patients with previous venous thromboembolism.7
Management
The main treatment for CVST is anticoagulation. Unfractionated heparin and low-molecular-weight heparin are most commonly used. Patients will also require long-term anticoagulation with an oral anticoagulant, such as warfarin, with a goal international normalized ratio of 2.5. Recommendations include treatment for three months in patients whose CVST was due to a transient risk factor, six to 12 months in those with idiopathic CVST or mild thrombophilia (eg, heterozygous factor V Leiden or prothrombin G20210A mutation and high plasma levels of factor VIII), and indefinitely in those with recurrent CVST or severe thrombophilia (eg, antithrombin, protein C, or protein S deficiency; homozygous factor V Leiden or prothrombin G20210A mutation; antiphospholipid antibodies; or combined prothrombotic conditions). Endovascular mechanical disruption of clots and direct thrombolysis are usually reserved for patients failing anticoagulation. Symptomatic treatment of elevated intracranial pressure and herniation can be approached with traditional methods. There has been no evidence to support glucocorticoid use. Symptomatic and prophylactic usage of antiepileptics are recommended in patients with higher risk of seizure (eg, supratentorial lesion involvement) and seizure on presentation. Valproic acid is commonly used due to fewer drug-to-drug interaction with anticoagulants.7
Case Resolution
Our patient was started on a heparin drip of 25,000 units in 500 mL 0.45% NaCl continuous infusion via our low-dose protocol without bolus and admitted to the neurology ICU, where she was bridged to warfarin and discharged five days later. On the evening of her discharge, the patient developed an acute five- to 10-minute episode of transient left arm stiffening, paresthesias, uncontrolled cramping of her left fingers, and worsening of her left facial droop, which were thought to be focal seizures due to the location of her CVST in combination with a family history of seizure disorder. She was admitted to the neurology service overnight for observation and discharged on levetiracetam 750 mg every 12 hours. At three months postevent, the patient had no recurrence of seizures or stroke-like symptoms and remained compliant with her coumadin and levetiracetam.
Pages: 1 2 | Single Page




One Response to “How to Spot and Treat Cerebral Venous Sinus Thrombosis”
March 1, 2021
MaxineWhat is meant by and treatment for assymetrical blood flow to venous sinuses tell me about it