A few statistics that help to frame our hospital capacity crisis today: Immediately following World War II, the population of the U.S. was 144 million and there were more than 1 million inpatient hospital beds. Today, the U.S. population has more than doubled to 336 million, but hospital beds have been reduced to 917,000. Simply put, there are not enough inpatient beds in this country.
Explore This Issue
ACEP Now: Vol 43 – No 03 – March 2024Prior to 2020, the problem of boarding, the holding of admitted patients in the emergency department (ED), was beginning to show signs of being managed. The Emergency Department Benchmarking Alliance (EDBA) had noted that pre-pandemic boarding, captured and measured as Admit Decision to Departure (ADD) time, was trending downward.1 Many hospitals and EDs during the pandemic actually got a brief reprieve in terms of their volumes. Most however are now seeing their volumes roaring back alongside the concomitant return of extreme levels of boarding. To the horror of the front-line doctors and nurses, these extreme boarding conditions come with all of the poor outcomes and sequelae we expect to accompany hospital boarding in the ED.2-5
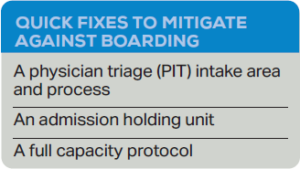 There are several quick fixes that can mitigate boarding. Two are in the front end and two in the back end. The first fix in the front end allows EDs of all sizes to continue to manage patients, even when much of the department’s real estate and resources are given over to the care of admitted patients. This initiative involves creating a Physician in Triage (PIT) model or more accurate nomenclature would be a “Physician Intake” area.6-8 PIT initiatives have been found to reduce wait times to see the physician, reduce walkaways, increase patient satisfaction and improve the quality of care for patients with time-dependent conditions.9-12 PIT is no longer a fringe idea. Many consider it a best practice, and the majority of moderate- to high-volume EDs in the U.S. employ a variation of this process.1
There are several quick fixes that can mitigate boarding. Two are in the front end and two in the back end. The first fix in the front end allows EDs of all sizes to continue to manage patients, even when much of the department’s real estate and resources are given over to the care of admitted patients. This initiative involves creating a Physician in Triage (PIT) model or more accurate nomenclature would be a “Physician Intake” area.6-8 PIT initiatives have been found to reduce wait times to see the physician, reduce walkaways, increase patient satisfaction and improve the quality of care for patients with time-dependent conditions.9-12 PIT is no longer a fringe idea. Many consider it a best practice, and the majority of moderate- to high-volume EDs in the U.S. employ a variation of this process.1

Example of a PIT, or physician intake area, space at a hospital.
When boarding is prevalent in a department, the physicians caring for those boarders will likely have the capacity to see new patients. The physicians have capacity (meaning time, medical knowledge and energy) but no place in which to see new patients. By creating a properly resourced intake area, arriving patients can continue to be seen and managed by physicians.
A PIT area (or physician intake area) typically needs an exam space with an exam table or stretcher, a computer for documentation and order placement, a workspace for an ED Technician to take vital signs and draw blood, supplies for this front-end work (i.e., phlebotomy and urine collection) and a waiting area for vertical patients to wait for test results. Some PIT models have a small medication-dispensary system for limited medication administration.




One Response to “Survival Tactics for Emergency Department Boarding”
March 10, 2024
Todd B Taylor, MD, FACEPThank you Shari. Your contribution to addressing this & other serious healthcare issues over the years has been laudable.
The failure of inpatient bed capacity to keep up with population is stark, albeit sameday outpatient surgery with new techniques have changed a 2-day hospital stay into a long afternoon in post-op. And, changes in healthcare funding policy has forced hospitals & others to dramatically change business practices.
In Arizona, in the late 1990’s to late 2000’s the Arizona ACEP Chapter had a huge impact on hospital crowding, to which you alluded.
But, now, here we are again & what appears to be worse & more wide-spread. So once again, the Arizona Chapter Board is taking action to draw attention to & impact this serious issue.
This time, we have chosen to employ data (not readily available in the past) to incentivize hospitals to take appropriate action & join with the EM community to lobby for policy changes. Anyone interested may contact me for a summary.
Thanks again for summarizing this timely topic.