A Primer on Boarding for the ED Physician
While the problem of boarding plays out in the ED, the real solutions to boarding are on the inpatient side and they are not simple. They often require culture change along with sweeping operational changes. The emergency physician ought to have some understanding of the basics of hospital boarding and its hospital-side solutions. The problem of boarding is due to a demand-capacity mismatch.19 This is most notably related to high census combined with inpatient discharge delays.20,21 Thirty years ago hospitals often operated at less than 90 percent capacity. In this new era of capacity constraint many large hospitals operate at 110 percent capacity or higher, with the continual boarding of inpatients in the ED and post-op spaces. For every patient being discharged there is already a patient waiting to take their place. If the discharge is delayed that patient remains in limbo, ergo boarding in the ED.
Explore This Issue
ACEP Now: Vol 43 – No 03 – March 2024By day of the week and hour of the day, most hospitals are in a state of perpetual disequilibrium. Admissions outpace discharges; and then on weekends there is a catch-up phenomenon.
Demand is so tight relative to capacity that any delay in discharging a patient translates into boarding. Innovative hospitals have been addressing disequilibrium by focusing on the capacity side of the equation, creating or optimizing capacity one initiative at a time.
Most tactics that provide remedies to alleviate boarding do so by creating or recovering inpatient capacity. They do this by either improving throughput or addressing discharge delays.22-30 Much work has been done by hospitalists, who are now the largest admitting service at most hospitals (and the majority of patients boarding in the ED are general-medicine admissions). The emergency physician should have a passing knowledge about the remedies and inpatient best practices for throughput and discharge.
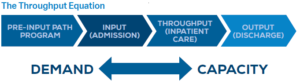 Unfortunately, pent-up demand for health care services deferred during COVID-19 has wiped out the capacity gains that hospitals had been making. A profound capacity crisis is afoot, and most EDs are experiencing boarding levels never seen before. Stakeholders are exploring any tactics to further address or mitigate boarding. Attention is shifting to the demand side of the equation, with a focus on “avoidable admissions.”31,32 Avoidable admissions for a group of diagnoses known as ambulatory care sensitive conditions (ACSC) are thought to be preventable. With the provision of timely and effective ambulatory-care services, many conditions can be treated as outpatient illnesses and the hospitalization avoided.
Unfortunately, pent-up demand for health care services deferred during COVID-19 has wiped out the capacity gains that hospitals had been making. A profound capacity crisis is afoot, and most EDs are experiencing boarding levels never seen before. Stakeholders are exploring any tactics to further address or mitigate boarding. Attention is shifting to the demand side of the equation, with a focus on “avoidable admissions.”31,32 Avoidable admissions for a group of diagnoses known as ambulatory care sensitive conditions (ACSC) are thought to be preventable. With the provision of timely and effective ambulatory-care services, many conditions can be treated as outpatient illnesses and the hospitalization avoided.





One Response to “Survival Tactics for Emergency Department Boarding”
March 10, 2024
Todd B Taylor, MD, FACEPThank you Shari. Your contribution to addressing this & other serious healthcare issues over the years has been laudable.
The failure of inpatient bed capacity to keep up with population is stark, albeit sameday outpatient surgery with new techniques have changed a 2-day hospital stay into a long afternoon in post-op. And, changes in healthcare funding policy has forced hospitals & others to dramatically change business practices.
In Arizona, in the late 1990’s to late 2000’s the Arizona ACEP Chapter had a huge impact on hospital crowding, to which you alluded.
But, now, here we are again & what appears to be worse & more wide-spread. So once again, the Arizona Chapter Board is taking action to draw attention to & impact this serious issue.
This time, we have chosen to employ data (not readily available in the past) to incentivize hospitals to take appropriate action & join with the EM community to lobby for policy changes. Anyone interested may contact me for a summary.
Thanks again for summarizing this timely topic.