Explore This Issue
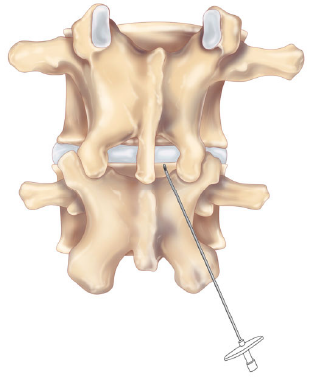
ACEP Now: Vol 36 – No 06 – June 2017Figure 1: Posterior view of the lumbar spine.
Lumbar puncture is an essential skill for emergency physicians and the gold standard diagnostic procedure allowing for the rapid analysis of cerebrospinal fluid (CSF) to rule out dangerous conditions such as meningitis, subarachnoid hemorrhage, and other neurologic conditions.1 In our busy departments, lumbar puncture failure can be frustrating and time-consuming and cause added stress to clinicians and patients. A successful lumbar puncture demands an intricate knowledge of anatomy, positioning, and technique. Without this experience and knowledge, we are left to rely on anatomical landmarks that can be misleading in more than 30 percent of people requiring the procedure. Obesity is a common challenge we face; it makes landmark acquisition and positioning difficult if not impossible.2 Additional challenges include age-related anatomical changes, such as the calcification of the interspinous ligaments, which can complicate needle insertion, causing deflection of the needle and increased pain.3
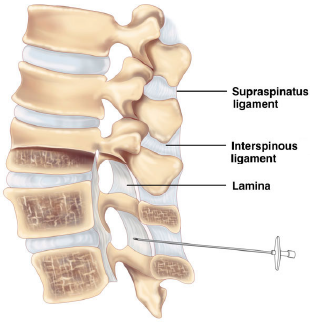
Figure 2: Lateral view of the lumbar spine.
Images courtesy of EMSONO (emsono.com)
As emergency physicians, we have been trained to always have a backup plan and an alternative approach for all procedures. However, if the midline approach fails at a particular level, most physicians will attempt the procedure using the same technique at another level. If this fails, the patient will frequently undergo a fluoroscopically guided or ultrasound-assisted lumbar puncture. This is likely because most emergency physicians have not been trained in an alternative approach to the lumbar puncture.
An alternative method to the traditional lumbar puncture is the paramedian approach. Although scarce in the emergency medicine literature, it has been a successful option that has been performed by anesthesiologists for decades. Advantages of this approach include a larger target through the interlaminar space as well as avoidance of the supraspinous and interspinous ligaments. The paramedian approach allows for faster catheter insertion, fewer attempts at needle insertion, and a lower incidence of post lumbar puncture headache.4-5 This approach can be performed in the neutral spine position.3 The paramedian approach is associated with fewer technical problems compared to the midline approach, and because it avoids the supraspinous and interspinous ligaments, the procedure is less painful and ideal in elderly patients with calcified ligaments. This approach penetrates the ligamentum flavum directly after passing through the paraspinal muscles.6 First-attempt success rates with the paramedian approach have been reported to be 30 percent to 40 percent higher when compared to the midline approach.3
Paramedian Approach Technique
- Prepare your lumbar puncture kit. You will use the same equipment, positioning, local anesthesia, and sterile technique as you would for the midline approach. A longer spinal needle may be required since you are approaching the subarachnoid space at an angle.
- The patient can be positioned in the lateral recumbent or sitting position. Flexing the patient is not necessary using this approach.
- Identify the L4 spinous process by using the iliac crest as a landmark. Identify the caudal tip of the L4 spinous process and move your finger 1 cm inferior and lateral. Needle insertion will be in a cephalad and medial direction, with the needle angled 10°–15° toward the midline and 10°–15° in the cephalad direction. If contact is made with the lamina, the needle should be adjusted in a cephalad direction so that you are walking up the bone until you enter the subarachnoid space and obtain the CSF. (See Figures 1 and 2.)
Needle path: skin » superficial fascia » fat » erector spinae muscle » ligamentum flavum » subarachnoid space.
Pages: 1 2 | Single Page




3 Responses to “Techniques for Performing Paramedian Approach to Lumbar Puncture”
June 18, 2017
C TPlease note that “Tintinalli” in Reference 1 is misspelled.
June 23, 2017
Dawn Antoline-WangThank you, I have corrected the misspelling.
February 22, 2023
AHBThanks for the article.